Deep vein thrombosis (DVT)—the formation of a blood clot in a deep vein—and pulmonary embolism (PE)—a blood clot that travels to the lungs—together comprise the most common preventable cause of hospital-related death. Known together as venous thromboembolism (VTE), they claim more than 100,000 lives a year in the United States.
There is strong evidence that anti-clotting medications and mechanical prophylaxis, such as compression devices, can prevent a majority of blood clots in the hospital. Yet blood clot prevention is truly complicated. Prescribers must tailor prophylaxis to the individual patient, by considering risk factors and contraindications. Studies have found that appropriate prophylaxis is ordered for only 32 percent to 59 percent of patients. Additionally, an emerging body of research shows that once prophylaxis is ordered, treatments often do not reach patients.
Why Focus on VTE Prevention?
- VTE is common. There are an estimated 350,000 to 900,000 new cases annually in the United States during or after hospitalization. An additional 1 million estimated VTE cases are not related to hospitalization.
- VTE is deadly. Patients with a pulmonary embolism, when a blood clot travels to the lungs, have a 30 percent to 60 percent to chance of dying from it. Lower-extremity DVT has a 3 percent mortality rate, associated with blood clots that travel from the legs to the lungs.
- VTE is preventable. Best practice prophylaxis reduces VTE incidence by an estimated 70 percent.
- VTE frequently has complications. As many as 60 percent develop conditions such as postthrombotic syndrome, a long-term complication that causes pain, swelling, discoloration and, in serious cases, ulcers in the affected limbs.
- VTE is recurrent. Between 10 percent and 30 percent of people who survive an initial VTE develop another one within five years.
- VTE treatment is costly. Each DVT costs $10,000 and each PE costs $16,000, according to the Agency for Healthcare Research and Quality.
See our Strategies for Venous Thromboembolism Prevention
VTE FAQs
Content from the handout is adapted below.
-
Blood clots are called venous thromboembolisms (VTE). There are two main types:
- Deep vein thrombosis (DVT) is a clot in a deep vein, usually an arm or leg
- Pulmonary embolism (PE) is a clot that has broken off and traveled to the lungs. This can cause death.
-
VTE kills over 100,000 people every year in the United States. This is more than the number of deaths caused by AIDS, motor vehicle collisions and breast cancer combined.
VTE can cause problems that may affect you for the rest of your life. You may have:
- long-term problems with breathing
- a higher chance of getting another clot
- swelling that will not go away
- sores or wounds that will not heal
-
Some people who have VTE may not have any symptoms.
People with DVT may have the following in an arm or leg:
- swelling
- pain or cramping
- redness, tenderness or warmth
People with PE may experience:
- shortness of breath or are unable to catch their breath
- pain in the rib cage area
- coughing up blood
-
People who are in the hospital have a higher chance of getting a VTE. Other things that raise your chance of getting a clot:
- previous DVT/PE
- major surgery
- trauma
- obesity
- recent stroke
- family history of VTE
- bedrest
- varicose veins
- blood diseases
- pregnancy
- cancer and/or chemotherapy
- birth control pills and/or hormone replacement therapy
-
Depending on your situation you may have:
- a blood test called a D-Dimer
- an ultrasound of the arm or leg to look for the DVT
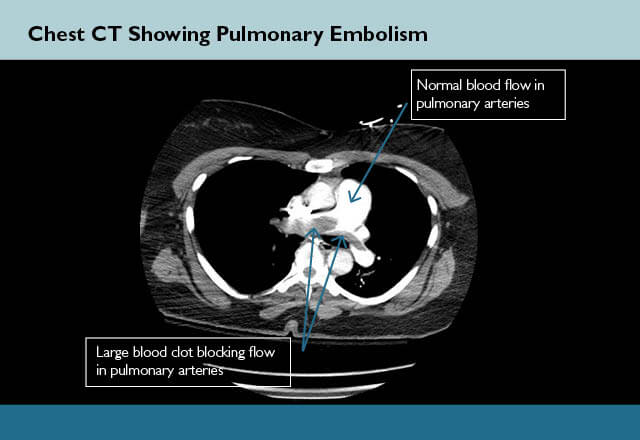
- a CAT scan of the chest with intravenous dye to look for PE
-
When you come to the hospital, the care team will look at all the risks you may have to get a clot. They then order what is best for you, to help stop a clot from starting.
- Medicines are the best way to stop a clot from forming. The 2 main medicines that are used to help prevent clots are heparin and enoxaparin (Lovenox). Some people call them blood thinners. These are shots that will be given to you usually in the belly.
- Special stockings also can help prevent clots. Sequential Compression Devices (SCDs) use a machine and squeeze the legs or feet gently. They need to be on as much as possible to help prevent clots. You may also be ordered compression stockings or TED hose. These also help with blood flow.
Although many people think walking around prevents blood clots, this is not true. Moving around and walking are important to keep you well and can help prevent things like pneumonia and bedsores. Walking by itself does not prevent clots. This is why your care plan should also include medications and/or SCDs and/or compression stockings your care team has ordered.
-
Depending on your specific condition you may need:
- an IV medicine such as heparin
- to take shots such as enoxaparin (lovenox)
- to take pills such as warfarin (Coumadin), rivaroxiban (Xarelto), or dabigatran (Pradaxa)
- to take these medicines for months or possibly your whole life
- to wear special stockings such as TEDs which can decrease your risk of long term problems that can be caused from having clots
- a special filter placed in a vein to “catch” the blood clot if it breaks free. Many of these can be removed after the danger from these clots have passed
-
- Educate and Learn in the same minute. Listen to VTE collaborative team member and nurse educator, Dauryne L. Shaffer, share her experience with educating patients about VTE.
- Watch videos
-
Video Gallery
How Do I Prevent Blood Clots?
Blood clots claim more over 100,000 lives yearly in the United States. Yet as serious a health issue as blood clots are, studies have shown at-risk patients often don’t receive treatments known to help prevent them.
National Blood Clot Alliance Stop the Clot
The National Blood Clot Alliance (NBCA) is a non-profit, voluntary health organization dedicated to advancing the prevention, early diagnosis and successful treatment of life-threatening blood clots such as deep vein thrombosis, pulmonary embolism and clot-provoked stroke.
Our Team
Formed in 2005, the Venous Thromboembolism (VTE) Collaborative provides evidence-based standards for venous thromboembolism risk assessment, ordering and administration of patient-specific prophylaxis, while also advancing the science of blood clot measurement. Members include a hematologist, trauma surgeon, pharmacist, clinical informatician, intensive care nurse, nurse educator, medical writer/editor, human factors engineer and researchers.
- Elliott Haut, M.D., Ph.D., F.A.C.S., Vice-Chair Quality, Safety and Service, Associate Professor of Surgery and Anesthesiology/Critical Care Medicine and Emergency Medicine, Johns Hopkins University School of Medicine; Core Faculty, Armstrong Institute for Patient Safety and Quality, Twitter: @ElliottHaut
- Deborah B. Hobson, B.S.N., M.S.N., Safety and Quality Improvement Specialty in Surgery, The Johns Hopkins Hospital
- Chris G. Holzmueller, B.L.A., Medical Writer/Editor, Division of Acute Care Surgery, Department of Surgery, The Johns Hopkins Hospital
- Brandyn D. Lau, M.P.H., C.P.H., Assistant Professor of Radiology and Radiological Science, Clinical Informatician at The Johns Hopkins University School of Medicine; Associate Faculty, Armstrong Institute for Patient Safety and Quality Twitter: @LauzeeTweet
- Oluwafemi P. Owodunni, M.D., M.P.H., Post-Doctoral Research Fellow, Division of Acute Care Surgery, Department of Surgery, The Johns Hopkins Hospital, Twitter: @Femiowodunni
- Dauryne L. Shaffer, M.S.N., R.N., C.C.R.N., Nurse Educator, Department of Surgery, The Johns Hopkins Hospital
- Michael B. Streiff, M.D., F.A.C.P., Associate Professor of Medicine and Pathology, Johns Hopkins University School of Medicine; Associate Faculty, Armstrong Institute for Patient Safety and Quality
- Mujan Varasteh Kia, MPH, Research Assistant, Division of Acute Care Surgery, Department of Surgery, The Johns Hopkins Hospital
- Kristen L.W. Webster, Ph.D., Post-Doctoral Research Fellow, Human Factors Engineer, Division of Acute Care Surgery, Department of Surgery, The Johns Hopkins Hospital, Twitter: @LiseWelsh
News and Publications
Regularly featured in national media, the following is a collection of the outlets where the VTE Collaborative has helped advance public knowledge on blood clot prevention and measurement.
-
- Recipient of 2019 E. Robert Feroli Award for Excellence in Medication Safety
- Getting patients on board with VTE prophylaxis (ACP Hospitalist, February, 2019)
- Taking bias out of health care (Heart & Stroke 2018 Heart Report)
- ‘Active learning’ module improves VTE prophylaxis administration (HemOnctoday, December 28, 2017)
- These 8 Groups Of People Are More Prone To Blood Clots (Prevent/Health, November 14, 2017)
- Toward More Personalized Learning (Johns Hopkins University School of Medicine, Fall edition, 2017)
- Preventing VTE takes a data-driven team effort (Clinical Congress Daily Highlights, Wednesday Second Edition, October 25, 2017)
- Online Education Boosts Proper Use of Drugs That Prevent Blood Clots (Press Release Point, August 17, 2017)
- Online education boosts proper use of drugs that prevent blood clots (Johns Hopkins University School of Medicine, August 16, 2017)
- Two more Senate Republicans oppose health-care bill, leaving it without enough votes to pass (The Washington Post, July 18, 2017)
- Inferior Vena Cava Filter Use Fell After FDA Warning but Remains High (tctMD/the heart beat, July 12, 2017)
- Becker’s Infection Control & Clinical Quality. 10 Most popular stories, studies on bloodstream infections and blood clots in 2015 (December 16, 2015)
- Surgeon-in-Training Report Cards Can Help Reduce Blood Clots in Hospitalized Patients. The Johns Hopkins News Media (Release Date: December 10, 2015)
- Blood Clots Show Limits of Quality Care Penalties (The Health Care Blog, August 6, 2015)
- Blood Clot Prevention Is Higher Priority at Hospitals (The Wall Street Journal, August 3, 2015)
- Bioscience Technology. Johns Hopkins Medicine. Scientific Daily. A Better Way to Prevent Blood Clots? (Release Date: October 15, 2012)
- After Hospital Discharge, Trauma Patients Face Increased Death Risk (AARP Bulletin, March 9, 2011)
- American College of Surgeons. Inspiring Quality: Leading the Way to Improve Care (ACS, Maryland Health Care Leaders Highlight Quality Improvement, 2011)
-
Below is a selection of several published articles that reflect the impact of the VTE Collaborative and the breadth of its research and improvement work. See an annotated bibliography for a full listing of more than 50 articles by the collaborative.
Most Cited Publications
- Haut E.R., Pronovost P.J. Surveillance Bias in Outcomes Reporting. JAMA – J Am Med Assoc. 2011; 305(23):2462-3.
Mini-abstract: This article tries to draw attention to the significant risk of surveillance bias inherent in measurement of performance through reported outcome measures in the absence of standardized surveillance. - Segal J.B., Streiff M.B., Hofmann L.V., Thornton K., Bass E.B. (2007). Management of venous thromboembolism: A systematic review for a practice guideline. Annals of Internal Medicine, 146(3), 211-222.
Mini-abstract: This articles reviewed the evidence on the efficacy of interventions for treatment of deep venous thrombosis (DVT) and pulmonary embolism. - Pierce C.A., Haut E.R., Kardooni S., Chang D.C., Efron D.T., Haider A., Pronovost P.J., Cornwell E.E. 3rd. Surveillance bias and deep vein thrombosis in the national trauma data bank: The more we look, the more we find. J Trauma. 2008;64(4):932-6; discussion 936-7.
Mini-abstract: The results of this study indicate that hospital DVT rate has a positive association with hospital duplex rate among trauma centers in the NTDB. It provides further evidence that hospital DVT rate is a poor quality indicator in trauma because of the presence of surveillance bias - Streiff M.B., Carolan H.T., Hobson D.B., Kraus P.S., Holzmueller C.G., Demski R., Lau B.D., Biscup-Horn P., Pronovost P.J., Haut E.R. Lessons from the Johns Hopkins Multi-Disciplinary Venous Thromboembolism (VTE) Prevention Collaborative. BMJ 2012;344:e3935
Mini-abstract: This study describes the experience of the Johns Hopkins VTE Collaborative in implementing a prospective quality improvement program which featured a mandatory clinical decision support tool for VTE risk stratification and risk-appropriate VTE prophylaxis for all hospitalized adult patients. Implementation of the tool resulted in a marked increase in risk-appropriate VTE prophylaxis. - Haut E.R., Lau B.D., Kraenzlin F.S., Hobson D.B., Kraus P.S., Carolan H.T., Haider A.H., Holzmueller C.G., Efron D.T., Pronovost P.J., Streiff M.B. Improved Prophylaxis and Decreased Rates of Preventable Harm With the Use of a Mandatory Computerized Clinical Decision Support Tool for Prophylaxis for Venous Thromboembolism in Trauma. Archives of Surgery 2012;147(10):901-7.
Mini-abstract: This study was designed to evaluate the impact of a mandatory clinical decision support tool on compliance with prophylaxis for venous thromboembolism and VTE outcomes among admitted trauma patients. Implementation of this tool was found to significantly increase compliance with VTE prophylaxis and decrease the rate of preventable harm. - Haut E.R., Noll K., Efron D.T., Berenholz S.M., Haider A., Cornwell E.E. 3rd, Pronovost P.J. Can Increased Incidence of Deep Vein Thrombosis (DVT) Be Used as a Marker of Quality of Care in the Absence of Standardized Screening? The Potential Effect of Surveillance Bias on Reported DVT Rates. J Trauma. 2007; 63(5):1132-1137
Mini-abstract: This retrospective study was designed to determine whether or not the rate of DVT identification increases as the number of screening duplex examinations in trauma patients increase. - Streiff M.B., Haut E.R. The CMS Ruling on Venous Thromboembolism After Total Knee or Hip Arthroplasty: Weighing Risks and Benefits. JAMA – J Am Med Assoc. 2009; 301(10):1063-1065.
Mini-abstract: This article comments on the designation of deep venous thrombosis and pulmonary embolism after total knee arthroplasty and total hip arthroplasty to the list of never events. It argues that the CMS rule may have a number of unintended consequences that could cause additional harm to patients undergoing TKA and THA. - Haut E.R., Schneider E.B., Patel A., Streiff M.B., Haider A.H., Stevens K.A., Chang D.C., Neal M.L., Hoeft C., Nathens A.B., Cornwell E.E. 3rd, Pronovost P.J., Efron D.T. Duplex Ultrasound Screening For Deep Vein Thrombosis in Asymptomatic Trauma Patients: A Survey of Individual Trauma Surgeon Opinions and Current Trauma Center Practices. J Trauma. 2011; 70(1):27-34.
Mini-abstract: This study surveyed trauma surgeons to obtain opinions regarding duplex ultrasound screening for DVT in asymptomatic trauma patients. There was wide variation in trauma surgeons’ opinions and trauma centers’ practices regarding duplex ultrasound screening for DVT in asymptomatic trauma patients. - Streiff M.B., Brady J.P., Grant A.M., Grosse S.D., Wong B., Popovic T. CDC Grand Rounds: Preventing Hospital-Associated Venous Thromboembolism; Johns Hopkins Medical Institutions Anticoagulation Management Service. MMWR Morb Mortal Wkly Rep. 2014 Mar 7;63(9):190-3. PMID: 24598595 [PubMed - in process]
Mini-abstract: This Morbidity and Mortality Weekly Report provides an overview of the epidemiology and pathogenesis of venous thromboembolism and describes institutional efforts to improve venous thromboembolism prophylaxis at the Johns Hopkins Hospital, venous thromboembolism prevention as a component of patient safety and public health strategies to prevent venous thromboembolism. - Zeidan A.M., Streiff M.B., Lau B.D., Ahmed S.R., Kraus P.S., Hobson D.B., Carolan H., Lambrianidi C., Horn P.B., Shermock K.M., Tinoco G., Siddiqui S., Haut E.R. Impact of a Venous Thromboembolism (VTE) Prophylaxis “Smart Order Set”: Improved Compliance, Fewer Events. American Journal of Hematology 2013;88(7):545-549.
Mini-abstract: The objective of this retrospective cohort study was to examine the impact of a “smart order set” on VTE prophylaxis and events in medical inpatients. The “smart order set” increased the prescription of risk-appropriate prophylaxis and reduced the number of symptomatic VTE episodes without increasing the frequency of VTE-prophylaxis associated major bleeding.
- Haut E.R., Pronovost P.J. Surveillance Bias in Outcomes Reporting. JAMA – J Am Med Assoc. 2011; 305(23):2462-3.
-
- Haut ER, Aboagye JK, Shaffer DL, Wang J, Hobson DB, Yenokyan G, Sugar ES, Kraus PS, Farrow NE, Canner JK, Owodunni OP, Florecki KL, Webster LW, Holzmueller CG, Pronovost PJ, Streiff MB, Lau BD. Effect of Real-time Patient-Centered Education Bundle on Administration of Venous Thromboembolism Prevention in Hospitalized Patients. JAMA Netw Open. 2018;1(7):e184741
Mini-abstract: In this controlled preintervention-postintervention comparison trial of 19 652 adult patients on medical and surgical units, nonadministration of venous thromboembolism prophylaxis significantly declined on units that received an intervention that combined an alert to a health educator about a missed dose of venous thromboembolism prophylaxis with patient education compared with control units. - Murphy PB, Vogt KN, Lau BD, Aboagye JK, Neil GP, Streiff MB, Haut ER. Venous Thromboembolism Prevention in Emergency General Surgery: A Review. JAMA Surg. 2018;153(5):479–486.
Mini-abstract: In this study we found that Operatively and nonoperatively treated EGS patients are at a comparatively high risk of VTE. Despite gaps in existing literature with respect to this increasing patient population, successful best practices can be applied. Best practices include assessment of VTE risk, optimal prophylaxis, and physician, nurse, and patient education regarding the use of mechanical and pharmacologic VTE prophylaxis and institutional policies. - Lau BD, Streiff MB, Pronovost PJ, Haut ER. Venous thromboembolism quality measures fail to accurately measure quality. Circulation. 2018;137(12):1278-1284.
Mini-abstract: We developed a rubric for defect-free VTE prevention, graded each organizational VTE quality measure, and found that none of the current VTE-related quality measures adequately characterizes VTE prevention efforts or outcomes in hospitalized patients.
- Haut ER, Aboagye JK, Shaffer DL, Wang J, Hobson DB, Yenokyan G, Sugar ES, Kraus PS, Farrow NE, Canner JK, Owodunni OP, Florecki KL, Webster LW, Holzmueller CG, Pronovost PJ, Streiff MB, Lau BD. Effect of Real-time Patient-Centered Education Bundle on Administration of Venous Thromboembolism Prevention in Hospitalized Patients. JAMA Netw Open. 2018;1(7):e184741
-
- Shermock K.M., Lau B.D., Haut E.R., Hobson D.B., Ganetsky V.S., Kraus P.S., Efird L.E., Lehmann C.U., Pinto B.L., Ross P.A., Streiff M.B. Patterns of non-administration of ordered doses of venous thromboembolism prophylaxis: implications for novel intervention strategies. Public Library of Science One (PLoS One) 2013;8(6):e66311.
Mini-abstract: This retrospective study was carried out to identify efficient intervention strategies based on patterns of non-administration of ordered VTE prophylaxis. Overall, 11.9% of doses were not administered. The small proportion of patients that missed multiple ordered doses accounted for a large majority of non-administered doses. - Haut E.R., Lau B.D. Chapter 28: Prevention of Venous Thromboembolism: Brief Update Review. In “Making Health Care Safer II: An Updated Critical Analysis of the Evidence for Patient Safety Practices.” March 2013. Agency for Healthcare Research and Quality, Rockville, MD.
Mini-abstract: This chapter reviews current practices in VTE prevention and approaches for improving rates of risk-appropriate VTE prophylaxis. - Lau B.D., Haut E.R. Practices to Prevent Venous Thromboembolism: A Brief Review. BMJ Quality & Safety. 2014; 23:187-95.
Mini-abstract: This article reviews the practices and interventions that have been directed towards improvement of VTE prophylaxis prescription in hospitals from 2001-2012 and assesses their efficacy. The authors recommend provider education and active mandatory tools such as computerized clinical decision support, combined with other interventions. - Lau B.D., Haider A.H., Streiff M.B., Lehmann C.U., Kraus P.S., Hobson D.B., Kraenzlin F.S., Zeidan A.M., Pronovost P.J., Haut E.R. Eliminating Health Care Disparities With Mandatory Clinical Decision Support: The Venous Thromboembolism (VTE) Example.Med Care. 2015 Jan;53(1):18-24
Mini-abstract: This retrospective study was designed to examine the effect of implementation of a computerized clinical decision support (CCDS) tool on race-based and sex-based health care disparities across two distinct clinical services. When the proportion of patients prescribed risk-appropriate, best-practice VTE prophylaxis was evaluated pre-implementation, there were racial disparities in compliance between black and white patients. However, implementation of the CCDS tool improved compliance with best-practice VTE prophylaxis prescription and racial disparities were eliminated. - Elder S.L., Hobson D.B., Rand C.S., Streiff M.B., Haut E.R., Efird L.E., Kraus P.S., Lehmann C.U., Shermock K.M. Hidden barriers to the delivery of pharmacologic venous thromboembolism prophylaxis: the role of nursing beliefs and practices. Journal of Patient Safety 2014 March
Mini-abstract: This study was designed to explore causes of variability in the rate of administration of ordered doses of pharmacological venous thromboembolism prophylaxis among nurses on 12 inpatient hospital units using mixed-methods. Findings from the study showed that nurses on units with low administration rates often believe they have the skills to determine which patients require pharmacological venous thromboembolism prophylaxis and are more likely to offer the medication as optional to patients.
- Shermock K.M., Lau B.D., Haut E.R., Hobson D.B., Ganetsky V.S., Kraus P.S., Efird L.E., Lehmann C.U., Pinto B.L., Ross P.A., Streiff M.B. Patterns of non-administration of ordered doses of venous thromboembolism prophylaxis: implications for novel intervention strategies. Public Library of Science One (PLoS One) 2013;8(6):e66311.