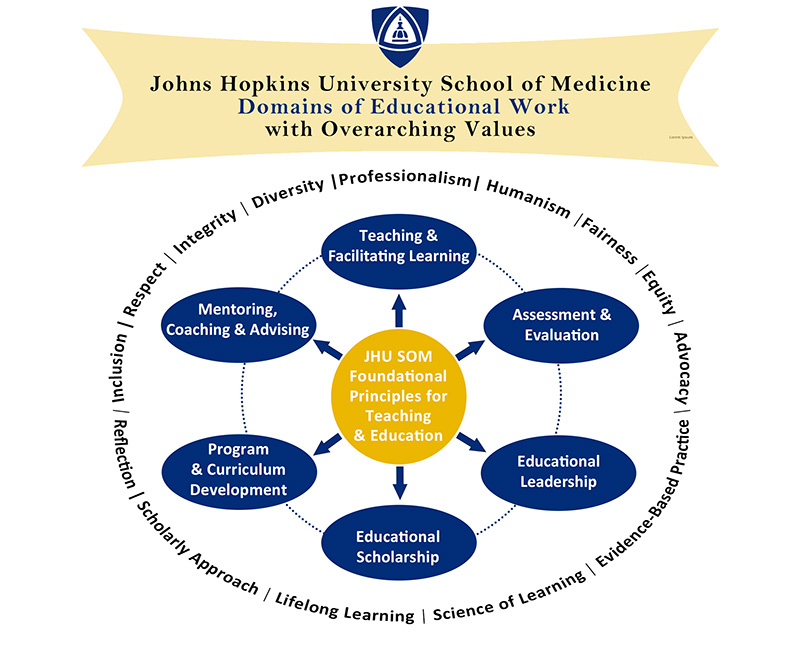
The mission of the Institute for Excellence in Education (IEE) is to promote, value and advance the educational mission of the School of Medicine while enhancing the school's leadership role in medical and biomedical education. To guide this mission, IEE has identified four guiding principles or "pillars" into which all of our decisions, work and programs are aligned.
For the 2023-2024 academic year, the IEE is highlighting the theme of “Successful Education: Thriving Learners, Flourishing Educators.”
Explore the Pillars of Our Mission
-
Pillar I
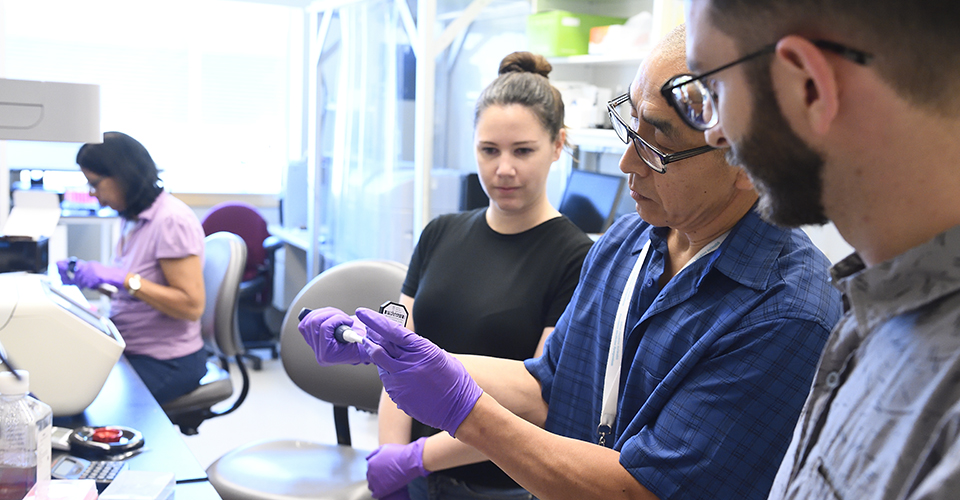
Improving Teaching

-
Pillar II
Inspiring and Supporting Research, Scholarship and Innovation in Education
-
Pillar III
Valuing and Recognizing Teachers and Educators

-
Pillar IV
Fostering a Community of Educators

IEE Calls to Action
Funding Opportunities
Apply for grant funding through our small grants program, the Faculty Education Scholars Program, or submit a proposal to be considered for IEE Education Shark Tank.
Nominations
The IEE Outstanding Educator Awards are designed to recognize and celebrate our outstanding educators and acknowledge great achievements in education. The awards are open to any full- or part-time faculty members of the School of Medicine, and are peer nominated, reviewed and selected.
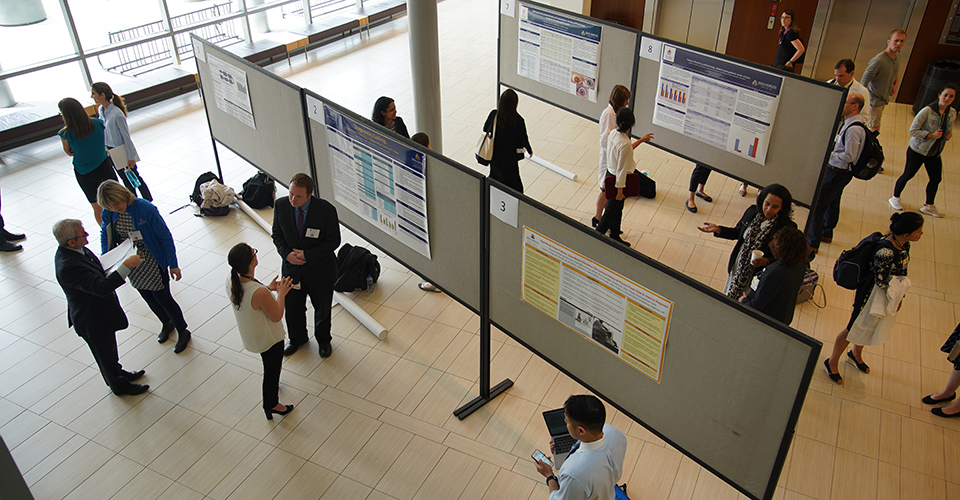
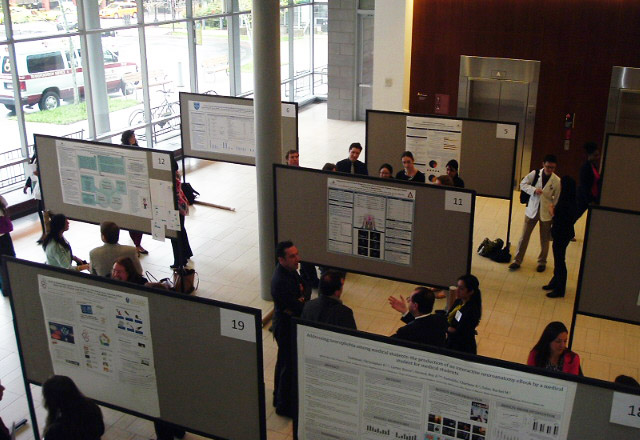
Present Your Scholarship
Submit a scholarship or innovation abstract to be considered for the upcoming IEE Education Conference and Celebration. We invite you to submit abstracts in all areas of medical, biomedical, nursing or public health education.
Upcoming Events
-
8 MAY 2024
Medical and Biomedical Education Grand Rounds
David Asai, PhD
4:00 - 5:00 pm
Basic Sciences Building -
26 JUN 2024
Medical and Biomedical Education Grand Rounds
Cornelius James, MD
4:00 pm - 5:00 pm
Armstrong Medical Education Building
Strauch Auditorium -
25 JUL 2024
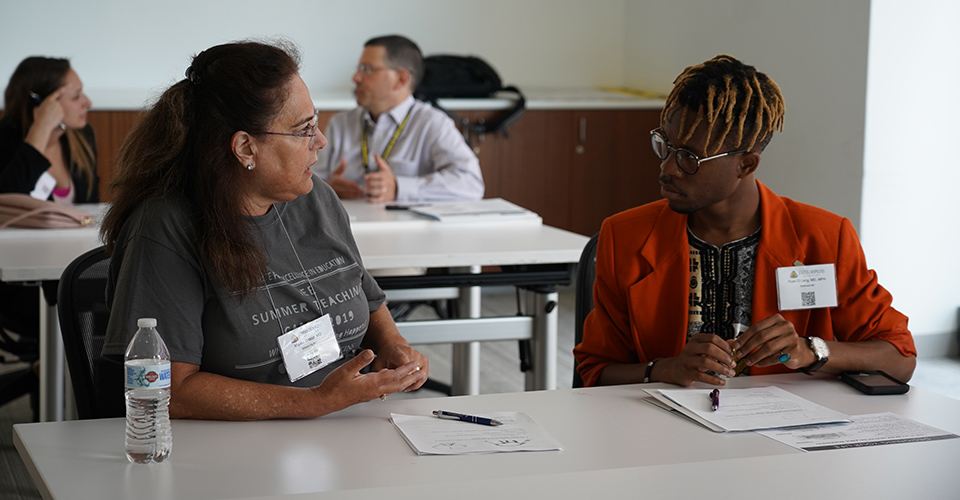
Summer Teaching Camp
9:00 PM - 5:00 PM
Armstrong Medical Education Building
REGISTRATION OPEN