Office of Well-Being Stories and Interviews
Our Interviews
H.O.P.E. Staff Stories
Vivian V. Altiery De Jesús (Bayview) | Serina Freeman (Home Care Group) | Michele Milord (JHCP) | Olivia Sutton (JHH) | Tracy Lowrey (Suburban) | Sheila Castle (All Children's) | Jean Deafenbaugh (Bayview) | Kassim Alli-Balogun (Home Care Group) | Julia Grossman (Suburban Hospital)
Vivian V. Altiery De Jesús, M.D., M.B.E.

PGY-2 Internal Medicine
Johns Hopkins Bayview Medical Center
Pandemic activity: Photography
I have always found photography fascinating. The ability to capture time itself in a moment and being able to cherish it for life. Dividing photos into collections, curating and taking new photos allowed me to connect with a dimension untarnished by the COVID-19 pandemic; it was a glimmer of hope to return to the world I once knew before.
How did your activity support you in believing there was hope?
Photography requires stillness and immersion. It helps me ground myself to the present and appreciate what surrounds us every day. It is a paradox of isolation yet connectedness with the world; a chance to capture the glimmer of hope that engulfs every one of us.
How did your activity help support you and help make sense of what you were going through?
Nature is my favorite theme. Its untamed beauty fosters a feeling of stability and belonging. A sense of normalcy amid the chaos. The camera lens and the process of creating the collection helps me appreciate the big sphere I call home.
Selected Photographs
Serina Freeman

Home Health Aide
Johns Hopkins Home Care Group
Pandemic Activity: Social media encouragement posts
How did the activity support you in believing there was hope?
I used social media and life experiences as a platform for a supportive morale booster. I would make daily posts directed to all Johns Hopkins Home Care Group field staff as we went out every day to do direct patient care. At that time, full PPE was required for every patient during patient care. In-home dynamics were apparent, and at that time all we knew was our health and safety were at stake. We were concentrating on keeping safe and not taking anything home to our families. I would always say, “We can do this better together” and “Always check on each other, you never know what kind of day we’re having.” I believe it is still working, as clinicians still comment on the posts and tell me in person, “Thank you for caring and supporting us.” This pandemic has brought us closer together in so many ways, and has shown us resilience: That we will get through this together!
How did your activity help support you and help make sense of what you were going through?
I get support from listening to others vent or cry, just encouraging them and letting them know we will get through this. None of this makes sense. I miss the hands-on contact, the touching, the hugging and just smiling. It has been two years since our patients have seen us smile. Facial expressions matter; they let our patients feel more safe and secure. Prayer is my lifeline, and it continues to be. I start my day off with prayer to help us make it through our day no matter what issues or decisions we have to make, and it ends my day. When I see that all the patients survived, then it was a very good day!
Michele Milord

Coding Specialist/ Education and Training (C-CARES TEAM)
Johns Hopkins Community Physicians
Pandemic Activity: sewing
How did your activity support you in believing there was hope?
I’ll say this much, “to everything there is a season.” I knew this too shall pass, I had hope that we would be able to go back to normal, and when we come out of the pandemic, the result will be it took a pandemic to motivate me to create a new habit. Making reusable grocery bags was a way for me to cope with the ongoing pandemic situation; however, the vaccine gave me hope that there is light at the end of the tunnel. At some point, I stopped keeping track of the daily deaths statistics because it was too depressing.
How did your activity help support you and help make sense of what you were going through?
Making reusable grocery bags helps me fight against the feelings of social isolation and loneliness. Sewing helps me stay in touch with a social network. I can use the bags to communicate with my family and friends, and in turn have received a plethora of great quality fabrics to complete projects. Instead of watching the news, I have spent more time looking for the right fabrics, improving my techniques, and researching different types of bags to make. I do all this with the motivation to show my family and friends that I care about them and that they are not alone during this tough time, while adding a personal touch to enhance their shopping experience.
Olivia Sutton
Anesthesiology and Critical Care Resident
The Johns Hopkins Hospital
Pandemic Activity: Created mosaics from medication vial caps
How did your activity help you believe there was hope?
My cap mosaic project allowed me to see color and beauty during the bleakest moments in the hospital. Even during the darkest moments, during patient codes or unprecedented situations requiring me to administer strong or uncommon medications, the thought of being able to save one piece of a tragedy for something beautiful gave me hope. Even more so, when my colleagues spotted me saving vial caps, many of them banded together and helped collect their own caps to give to me, which was really an especially beautiful gesture.
How did your activity help support you and help make sense of what you were going through?
The collection aspect became just as much an art and catharsis as the actual assembly of the caps into the final mosaic. I made my first piece as a self-portrait in the operating room as a reflection of all of our experiences, and I hope to complete more mosaics to reflect the other important aspects of the residency experience during COVID — interaction with colleagues and interaction with patients.
Olivia Sutton
Olivia Sutton saw beauty during the pandemic in the most unusual place: medicine vial caps.
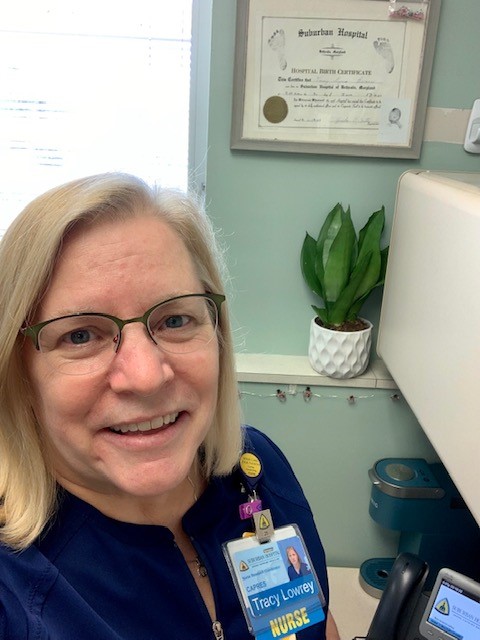
Tracy Lowrey, B.S.N., R.N.
Occupational Health
Suburban Hospital
Pandemic Activity: maintaining a Little Free Library
How did your activity support you in believing there was hope?
Maintaining the Little Free Library helped sustain my hope through the worst times of the pandemic. Having a focus outside of my extreme professional experience was grounding and refreshing. Sorting through book donations and monitoring the boxes was a daily therapeutic ritual. Seeing people just enjoying something so “normal” reminded me things in some ways ARE still normal. The kids learn about communities, sharing and that, despite the pandemic, the Little Free Library goes on. We added a play house, hula hoops, a corn hole game and a rope swing after our July Fourth outdoor event. These were so popular with the kids that we kept them out through the beginning of winter.
How did your activity help support you and help make sense of what you were going through?
Even my husband benefited — when teleworking, he had a view of the library, and happily reported our patrons’ activities at the end of the day. We had no idea how many parents, nannies and children (on foot or by bike or stroller) stopped by the library until telework began … and each and every visitor had a smile on their face. THERE we all see hope!
Sheila Castle, Clinical Supervisor

Vascular Access Team,
Johns Hopkins All Children’s Hospital
Pandemic Activity: Coloring
How did your activity support you in believing there was hope?
My coloring allowed me to concentrate on something happy and enjoyable. While coloring, thoughts of life returning to some sense of normalcy were possible. When I’m finished with a page, I feel such a sense of accomplishment!
How did your activity help support you and help make sense of what you were going through?
While coloring, I didn’t have to think about the problems of the world. I colored in my “Zen” room so I couldn’t hear the news on the television or the conversations of family members talking about the COVID pandemic.
Sheila Castle
When the pandemic forced everyone indoors, employees like Sheila Castle found creative ways to cope and to heal from the emotional impact.
Jean Deafenbaugh, B.S.N., R.N.

Float Nurse
Johns Hopkins Bayview Medical Center
Pandemic Activity: Making fleece blankets
How did your activity support you in believing there was hope?
I believe that reaching out to others helps me take the focus away from my circumstances. When I apply myself to a project that uplifts others, I can see the hope and joy of our future.

How did your activity help support you and help make sense of what you were going through?
By applying myself to the creation of these blankets for the NICU babies, I was able to feel a sense of purpose. Since I could not participate in my usual activities (church, choir, prayer group, community band … all of which had significant close contact), I could pour my energies into my blankets. Crocheting the edges is an easy task, which allows time to think. I am not sure there is any making sense of what we have gone through for the last two years, though I think there have been a lot of lessons learned and a tremendous amount of growth in us all because of the challenges the pandemic has presented to us. Being able to give to others hopefully has helped them feel supported and more able to cope during this difficult time.
Kassim Alli-Balogun

Home Care Nurse
Johns Hopkins Home Care Group
Pandemic Activity: Creating videos of patients’ pets
Pictures of myself and my patients’ pets or items gives me a form of relaxation therapy that I’m making a difference in myself, and they make patients more comfortable with the visiting nurse during the chaotic time. These activities are used for content for funny videos and distractions that support my beliefs that there’s hope and this too shall pass.
How did your activity help support you and help make sense of what you were going through?
The art of taking pictures and creating exciting video is a good stress release for my body, mind and soul. Being active and creative makes my body feel good, boosting my self-esteem and helping me concentrate as well as sleep well and feel better with what I’m going through in this pandemic time.
H.O.P.E.: Employees Share Healing Activities
Kassim Alli-Balogun, a home care nurse with Johns Hopkins Homecare Group, put smiles on his patients' faces during the pandemic by creating videos of their pets.
Julia Grossman
Suburban Hospital physician assistant, Julia Grossman knitted masks for others during the pandemic. Learn how her creative project helped her relax and relieve stress during that uncertain time.
How did your activity support you in believing there was hope?
I have always been a positive person, and fixing things or just making them better gives me great satisfaction. It is part of the reason I am a health care provider. As a physician assistant, working in the surgery and trauma services, I get to do this every day. I learned how to sew as a child, and I joined other colleagues in producing what was needed, and not available, at the beginning of the pandemic. Although resources were limited, I had enough fabric in my stash to make masks for family and friends, and particularly for several children who needed smaller sizes in order to go out with their parents.
As for knitting and planting flowers and vegetables (many from seed), I have done these things for many years. Hands in wool or alpaca, or soil, is very relaxing, and there is a certain joy that comes from transforming a ball of yarn into a hat, or a seed into a pepper, cucumber or beautiful flower bed. It was also fun to give some of these things away.
Small Grants
Won-Jung Hong (JHH) | Danie Noble (JHCP at Howard County Pediatrics) | Stephanie Al-Adhami (Howard County) | Ambereen Mehta (Bayview) | Kristin Moore (Howard County)
Won-Jung Hong, R.N.
RN, Maternal Fetal Medicine Clinic
Johns Hopkins Hospital
Small Grants Project: Various Activities to Support Social Connection and Well-Being for Maternal-Fetal Medicine Staff
Tell us about your project. What excited you the most? What are you most proud of?
The greatest benefit is that the project impacted the entire staff (nurses, patient service coordinators and certified medical assistants) positively and allowed us to focus on our well-being. I’m glad I had the opportunity to apply for the grant.
This project consists of three activities: relaxation, aromatherapy and wellness. Our first activity that we completed a couple of weeks ago was making aromatherapy roller balls. There were 14 different recipes, and individuals got to choose which recipes to use, including tummy tamer blends, muscle rub, focus, headache, clear skin and bug bite rollers. Aromatherapy can have a positive effect on health. It was very well received.
How has your project contributed to your team’s well-being?
Our office, like others in health care, has been through stressful times during the pandemic. Individually, everyone was dealing with their own issues. We give so much. Personally, it was hard to find time for myself. We give to our patients, our families. We needed something to help us focus on our own well-being. I heard about this grant and applied.
I had some collaboration on ideas and I had the support of my nursing team. We are so thankful for the money to fund this activity. One specific piece of feedback was that it was the best day ever.
What do you appreciate most about this opportunity?
It was very well received. There are people of all ages (on our team), but it seemed like an activity that everyone could participate in. You could find a recipe customized to your need. We did a pre- and post-activity stress test. We had 11 responses; two showed no change; two showed increased stress after; but seven showed reduced stress pre- and post-test. Communication with the well-being team has been good; the check-ins are helpful.
How did management support this project?
One of things I put in the grant application is that we were experiencing a change in management. Part of that process for me was knowing who to speak with. All of the managers were supportive. It took time to get it to the right person, but they were very supportive of it. It just took initiative to put in the time to get the approvals and submit the application. Our current manager is 100% supportive of this project. She has even contributed gifts and door prizes.
What did it mean to you that you got to choose your well-being project?
It was a really positive experience to be able to customize something specifically for our team and be supported in implementing it.
What advice do you have for someone starting a well-being project?
It was really helpful to get support and buy-in from different team members. Find out if the activity is something people really want, and get feedback on what would be good for the team. Collaborating on ideas can only make it better and make it a collective experience.
Danie Noble, R.N.

Practice Administrator
JHCP at Howard County Pediatrics
Small Grants Project: Provide an Arts-Based Team-building Activity Outside of Work
Tell us about your project. What excited you the most, and what are you most proud of?
I applied for the grant to do an art project with my team; basically, to take them to an art studio where we can do art together as a team, get out of the office, do something relaxing that didn’t require brain power, and enjoy each other’s company. There are 20 people on my team.
I wanted to pick a place close to the area of our practice so no one would travel far. I found an art studio where you go and they teach you how to paint. We picked a picture ahead of time that we all liked, and they walked us through step by step how to paint it. It was really nice — a couple of my staff even said this is so mindless that it’s soothing to do. It was just nice to have that downtime together because we’re with each other just as much as we’re with our families. We call each other our work family, and we never get the time to decompress and spend time together. It was just a really nice experience. The girl who taught the class was hilarious. It was lots of laughing, and laughter is the best medicine, right? We painted a big daisy, and everybody got to choose their background. It turned out neat because everybody’s daisy looked different. Some of my staff have their daisy hanging in the office.
I’m most proud of having a phenomenal team. It was neat when I did the survey questions and scores before the event, how high we scored. I was happy but worried if we could do better, but we did. It was good because our score did go higher. I’m biased. I have a wonderful team.
Next, we’re planning a pool party, which will include all the families: kids, spouses and significant others.
What motivated you to apply for the small grant?
I saw an email that was pushed out to us through one of our newsletters. I thought of the idea and jumped right on it. I actually had another boss at JHH when I worked downtown who used to take nurses to an art museum. I thought it was the perfect opportunity to do this with my team. I reflected on my experience, and thought it would be fun to do.
The application process was very easy. I applied and answered the questions. I pulled up research articles on art and how it can de-stress and added it to my application to back up my project and why I wanted to do it. I think that’s what helped me get the grant.
How has your project contributed to your team’s well-being?
I did a poll a week before we went to the event. I asked questions like “How stressed are you at work?” “How do you feel about working with your team?” and we scored them. Then we took the exact same poll a week after the event. It was drastically higher; it was neat to have the hard evidence.
What did it mean to you that you got to choose your well-being project?
I was super excited (when I was chosen). It was like winning an award. I felt validated in a way for what I wanted to do and that somebody else saw my vision and believed in it too. It was nice to have someone appreciate what I was trying to do.
Talk about getting leadership support for your project.
It was a challenge at first. Not so much for the activity, but because of time away from the office. I wanted to do it during a workday; that was important to me because I wanted everyone to participate and didn’t want to take away from people’s personal time. I wanted to close the clinic for a half-day, so I had to get buy-in. What we did, was some of the providers picked up a few extra sessions to make up for us closing early on that one half-day, and they all said it was worth it.
The cool thing is I had doctors, certified medical assistants, nurses and medical office assistants who went, so it was like the whole office went.
What advice do you have for someone starting a well-being project?
Take the time to do it. Do it for your team. It may take a minute from your day, but do it for your team. It’s so worth it.
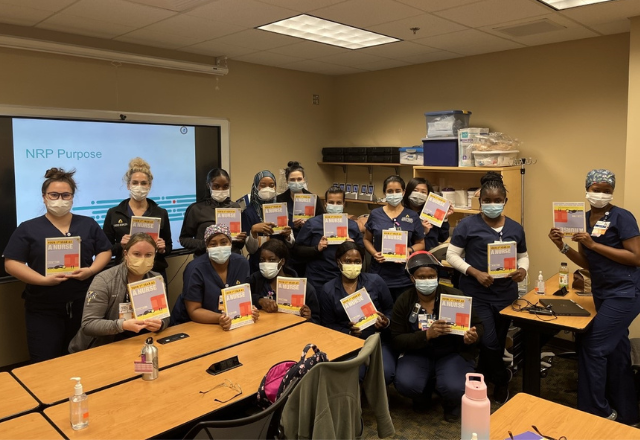
Stephanie Al-Adhami
Nurse Residency Program Manager (Educational Department)
Johns Hopkins Howard County Medical Center
Tell us about your project. What excited you the most, and what are you most proud of?
My project focused on the new graduate nurses. It was to start a book club for them. I gave a copy of Donna Cardillo’s book, Your First Year as a Nurse, to the new nurses when they started our residency program. We had one cohort start since we got the funds. Eighteen nurses have the book. The next cohort starts next month and they’ll receive the latest edition of the book.
What excited you most?
I think right now it’s tougher than it’s ever been to be a new graduate nurse. A lot of them had very limited in-hospital experience, if any really, during nursing school. So, they’re starting anew and figuring out what a hospital is and how it works. Everything is new to them. I thought this book could be one more resource to really help them with what was already a difficult transition — made 100 times worse by what they went through during the pandemic.
What made you apply for the grant?
We already do a lot of well-being initiatives here at HCGH. I was in the elevator one day and saw the flyer about grants. I started thinking: How could this help the group I’ll be working with? I think the new grads are in such a unique situation that nobody’s ever been in before. So, anything we can provide to them to help with that transition would be a good thing. I took the idea to my director. She loved it and asked how she could support it. I had a lot of help, too, from the grants liaison. They helped set us up with the publisher, and we’ll now get a 50% discount on the book.
Tell us about the grant application process.
The process was fairly simple. One question asked, “What areas of well-being will this impact?” I thought: This impacts almost every area of well-being. I kept having ideas of how things were related. It was enlightening.
What has been the reaction from the nurses?
Surprise and appreciation. The book teaches everything from how to learn from a preceptor to how to integrate an interprofessional team. So giving the nurses a copy means they’ll have a resource when they encounter these issues. We still encourage them to talk to their peers and leaders, but it’s nice to have something to refer to personally and immediately.
What advice would you give someone who’s applying for a grant?
Know your resources to help you out. You can have a great idea but not know how to bring it to fruition. Be comfortable reaching out to people. Step back and look at your idea from the 30,000-foot level. Don’t get too far down in the weeds. Step back and see the big picture. Then do it.

Ambereen Mehta, M.D., M.P.H.
Palliative Care Program, Department of Medicine
Johns Hopkins Bayview Medical Center
Small Grants Project: Expand Thrive by Design Program
Tell us about your project. What excited you the most, and what are you most proud of?
As part of the palliative care group, a huge component of what we do for our patients, ourselves, our families and our communities is self-care, with an emphasis on making sure the hard, emotional work we do is not wearing on us so much. We use a common metaphor of ‘empty your cup so that it may be filled.’ As part of that, we have a regular initiative called Thrive by Design. It’s a project that involves music, art and self-reflection, and it’s open to our team and students rotating with us. It’s something we’ve done the past couple years with other grants and support. We wanted to find a way to highlight the fundamental need for everyone to take care of themselves and to share with the greater community on a larger scale; that’s where the idea of self-care/artistic expression came from.
What motivated you to apply for the small grant?
My mentor and our program director, Dr. David Wu knew about the program, and encouraged us to apply.
How has your project contributed to your team’s well-being?
I think it’s multifactorial. In its own existence, it is a constant reminder we need to always thrive. And especially in medicine and health care, we don’t always carve out the time to do that. We always talk about it, but I think there is a necessity to design it and actually make it happen as opposed to leaving it up to the individual.
Part of the Thrive by Design program is Thrive by Arts. Within our palliative group, it helped us to take time out every month and refresh ourselves. We’ve done all sorts of ideas, like photography and oil painting. There is a local photographer who photographed people living on the street and used that methodology to share their stories. We had him come talk to us to remind us to connect with ourselves and connect with the people we care for — which includes each other. This helps us take a moment, pause and recover, and it gives us the opportunity to rejuvenate, remember why we’re doing what we do and better take care of our patients. It’s also a great model for the students who rotate with us. We especially involved our ICU social workers and floor social workers because we do a lot of family meetings with them, and we wanted to make sure we give back to them, recognizing that it’s not just the groups directly benefiting from our work but indirectly benefiting as well. We did a little bit of checking in, and I went around and met with everybody. They all felt like it was something different, and it took them out of their normal.

Tell us about the application process.
The prompts were very helpful, and we put it together fairly quickly. I emailed Paula Teague with questions, and she was very helpful. We had questions about the timing, and she was super nice about it.
What did it mean to you that you got to choose your well-being project?
It was so exciting! This is one of the first grants I received, and I was really excited about it. It was an easy process; it wasn’t too strenuous. The risk/reward is very good that way.
Talk about getting leadership support for your project.
Our whole team was awesome, behind it 100%; it was fairly easy for us as a group. It was good for us to explore and express how we wanted to put this together, and we had a willingness to work together. Our palliative care group had about five core team members working on it, then we had residents, fellows, social workers and leadership — so about 30 people in all.
What advice do you have for someone starting a well-being project?
1. If you have an idea, don’t be afraid to flush it out and really delve into it. Sometimes it helps to do that before you talk to other people — people will give input that might change your idea. Then get input from your friends.
2. Find one or two trusted colleagues who really understand the endpoint and goal, and who can help you fine tune it without taking away the excitement and authenticity of the project. This is cliché, but the more times you practice writing and trying and doing it, the more comfortable you’ll get with the process. And it’s OK to get no’s. I heard a lot of no’s. You get better each time.

Kristin Moore
Nurse Manager, Specialty Care Unit
Johns Hopkins Howard County Medical Center
Small Grants Project: Enhancements to recharge space for SCU
Ask Kristin Moore to describe Howard County Medical Center’s specialty care unit (SCU), and she’ll give a unique response: melting pot. For a busy staff, that means no two days are the same, due to the diversity of the patient population and their needs. One day they’re working with critically ill patients who need intubation, the next they’re helping patients check in or check out. There’s constant movement for this team, and Moore is proud of the work they do.
So, when Moore’s hardworking team requested some enhancements to their break room, including a television, she could not think of a better way to thank them than to turn the space into an oasis. “They wanted to feel like they’re away from the unit when they’re on break,” she said. “We wanted to find ways we could improve resiliency.” When she saw the Office of Well-Being’s announcement for Small Grants for Well-Being Projects, she jumped at the chance to apply and immediately thought of how she could use the money for her team.
The first step for Moore was to get leadership approval. “I talked to my director,” she said. “She encouraged it 100%.” Things moved quickly from there. While she waited for her acceptance, the hospital purchased a massage chair for each unit. The application process was easy. And when she received the grant funds, Moore supplemented the chairs with ultraviolet lights to help with seasonal depression. She purchased equipment for salt gardens, then added assorted teas and coffees, books, a fan, a foot massager and a massage therapy gun, all to create a peaceful atmosphere.
The new break room space has been a hit with the staff, says Moore. The response from her team has been a mix of gratitude and appreciation. She sees a change in the way they interact with patients and with each other. “I am most proud of them being excited about their new room and watching them show it off to other colleagues,” she offers. “Health care morale is so low. I enjoyed being able to do something for the team so they know it’s not always about work. Take your break; take your time.”
And to anyone who’s considering applying for a small grant or doing something to enhance their team’s well-being, Moore offers this: Just do it. “For your staff to see that you thought about them (it) goes a long way. Even if it takes some time … just do it. It really does make a difference.”







