-
Gail V. Berkenblit, MD PhD

- Associate Program Director for Ambulatory Education, Osler Medical Residency
- Associate Professor of Clinical Medicine
-
Erica Nicole Johnson, MD

- Program Director, Internal Medicine Residency Program, Johns Hopkins Bayview Medical Center
- Associate Professor of Medicine
-
Paul O'Rourke, MD MPH

- Assistant Dean for Medical Student Affairs, Johns Hopkins University School of Medicine
- Associate Professor of Clinical Medicine
Bedside Medicine Initiatives
Johns Hopkins has partnered with two other leading academic medical centers to study resident wellness and clinical skill and the factors in the training environment that support those values in a five-year, $1.8 million, American Medical Association grant-supported study. Working under the hypothesis that time spent in direct patient care improves communication, heightens clinical skill, and supports professional wellness, faculty from Johns Hopkins Hospital, Johns Hopkins Bayview Medical Center, University of Alabama-Birmingham, and Stanford University are investigating over a dozen measures in the post-graduate training environment as they "re-imagine residency" for the twenty-first century.
During each year of your residency, the grant will fund innovative ways to facilitate outstanding clinical education. These carefully designed initiatives focus on improving your skills in communication and physical exam and mirrors the attributes of some of the best clinician educators by:
Strengthening your bedside physical exam and ultrasound skills through the Bedside Teaching Initiative.

Trainees spend little time at the bedside in the modern academic hospital and often sense a decline in their physical exam skills as they matriculate through residency. The bedside teaching initiative is designed to increase the amount of time that trainees spend at the bedside practicing and honing their physical exam and ultrasound skills under the guidance of dedicated clinician educators. We believe increased time at the bedside will improve satisfaction and engagement in the educational environment and decrease burnout.
Providing you with direct, personalized feedback on how to improve your clinical skill through the Assessment of Physical Exam and Communication Skills (APECS) Initiative.

Assessment of Physical Examination and Communication Skills (APECS) is a novel assessment that uses encounters with both real and standardized patients to assess bedside clinical skills. APECS is modeled after the high-stakes MRCP (UK) Practical Assessment in Clinical Examination Skills (PACES) but includes real-time feedback and coaching from experienced faculty preceptors as part of a formative evaluation. During APECS, interns rotate through a series of stations where they encounter both real patients with real disease and standardized patients in the presence of a general internist and subspecialist. At the end of the series, residents receive personalized feedback on how to improve their clinical skills.
* Activities are modified for appropriate social distancing with masking during the COVID-19 pandemic and include telemedicine encounters.
Improving your communication and connection with patients through the Presence 5 Initiative.
The Stanford Presence 5comprises evidence-based practices that help foster clinician awareness, focus, and attention with the intent to understand and connect with patients. Presence 5 focuses on 5 important steps: preparing with intention, listening intently, agree on what matters, connecting with the patient’s story, and exploring a patient’s emotional cues. Presence 5practices help improve residents’ confidence in their interpersonal skills and experience meaningful interactions with their patients.
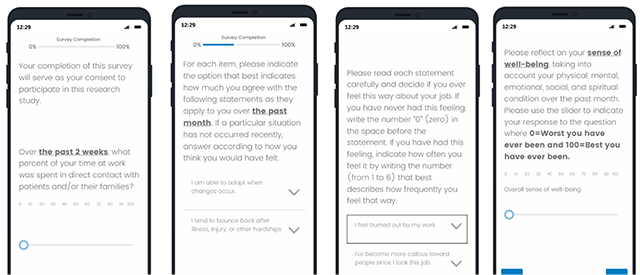
Assessing your residency experience, learning environment, wellness along the way through monthly surveys.
We believe your residency experience is deeply influenced by the learning environment and your wellness. We value your wellness and wellbeing. Using a variety of validated survey tools compiled into a monthly survey assessment, we assess residents’ sense of fulfillment, workload, and wellness. We use your feedback to inform and modify our initiatives aimed to help you.
Our Grant Team and Partners

Our Local Team
More Local Team Members
- Amanda Bertram, MS
- Ariella Apfel, MS
- Marielle Bugayong, MS
- Jenifer Hollett
- Bama Padmanaban
Publications Related to Clinical Skills
- Internal Medicine Intern Performance on the Gastrointestinal Physical Exam
- Use of a Real-Time Locating System to Assess Internal Medicine Resident Location and Movement in the Hospital
- Relationship of Physical Examination Technique to Associated Clinical Skills: Results from a Direct Observation Assessment
- Seven reasons why the physical examination remains important
- Strategies to Improve Bedside Clinical Skills Teaching
- Peabody's Paradox: Balancing Patient Care and Medical Education in a Pandemic
- Assessing physical examination skills using direct observation and volunteer patients
- The genealogy of teaching clinical reasoning and diagnostic skill: the GEL Study
- The Modern Physical Exam - A Transatlantic Perspective from the Resident Level
- Reinvigorating the clinical examination for the 21st century
- Strategies to Avoid the "Hemolyzed" Physical Examination
- Use of a Real-Time Location System to Understand Resident Location in an Academic Medical Center
- The physical examination, including point of care technology, is an important part of the diagnostic process and should be included in educational interventions to improve clinical reasoning
- The Hypothesis-Driven Physical Examination
- A novel bedside cardiopulmonary physical diagnosis curriculum for internal medicine postgraduate training
Contact
Brian T. Garibaldi, MD, MEHP
Associate Professor of Medicine and Physiology
[email protected]