Philosophy and History
Mission Statement
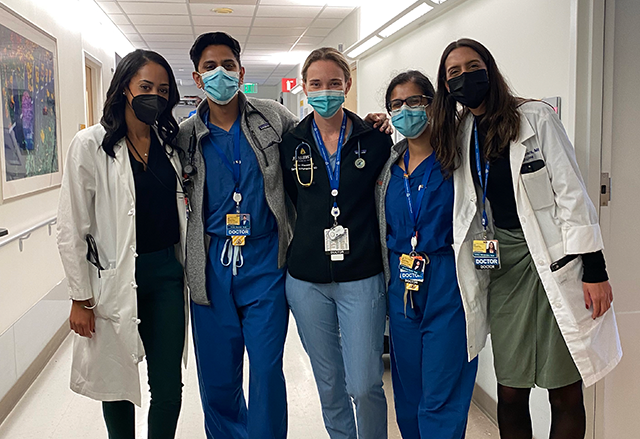
The Mission of the Osler Medical Residency is to develop preeminent leaders in medicine who have the skills to inform, manage, deliver, and shape healthcare. This encompasses leadership in all aspects of medicine, including clinical care, research, education, and public policy.
To this end, the program has seven specific aims:
- Prepare all trainees to practice exceptional ambulatory and inpatient care
- Ensure all trainees develop outstanding clinical skills
- Ensure all trainees can teach the medicine they practice
- Provide an inquisitive environment for scholarly pursuit and new discovery
- Facilitate training opportunities in science, public and global health, healthcare policy, and systems administration
- Engage and enable faculty to participate in the teaching mission
- Foster a learning environment rooted in respect that facilitates collaboration among all participants in the delivery of patient care
Aequanimitas

Aequanimitas is the motto of the Osler Program, and is part of our program philosophy. The term means “imperturbability” and was regarded by the first Chairman of our Department of Medicine, Sir William Osler, as the premier quality of a good physician.
In his essay, Aequanimitas, Osler further defined this concept as coolness and presence of mind under all circumstances, and “calmness amid storm, clearness of judgment in moments of grave peril.” In full development, it has the nature of a divine gift, a blessing to the possessor, a comfort to all who come in contact with them. At the beginning of their Osler residency, interns are given a copy of this essay.
Aequanimitas is displayed on the housestaff tie and scarves, which are given to incoming interns as an introduction and welcome to the family and tradition of our training program. The tie/bowtie/scarf is traditionally worn every Friday. This tradition has lived on at academic centers across the country where Osler alumni move beyond the dome.
History of the Department of Medicine
Sir William Osler, the first Chairperson and Physician-in-Chief of the Johns Hopkins Department of Medicine, was perhaps the most renowned physician of his time. A master clinician, author of the historic "Principles and Practice of Medicine," and a warm and gracious mentor, Osler attracted talented aspiring physicians to Johns Hopkins for medical training.
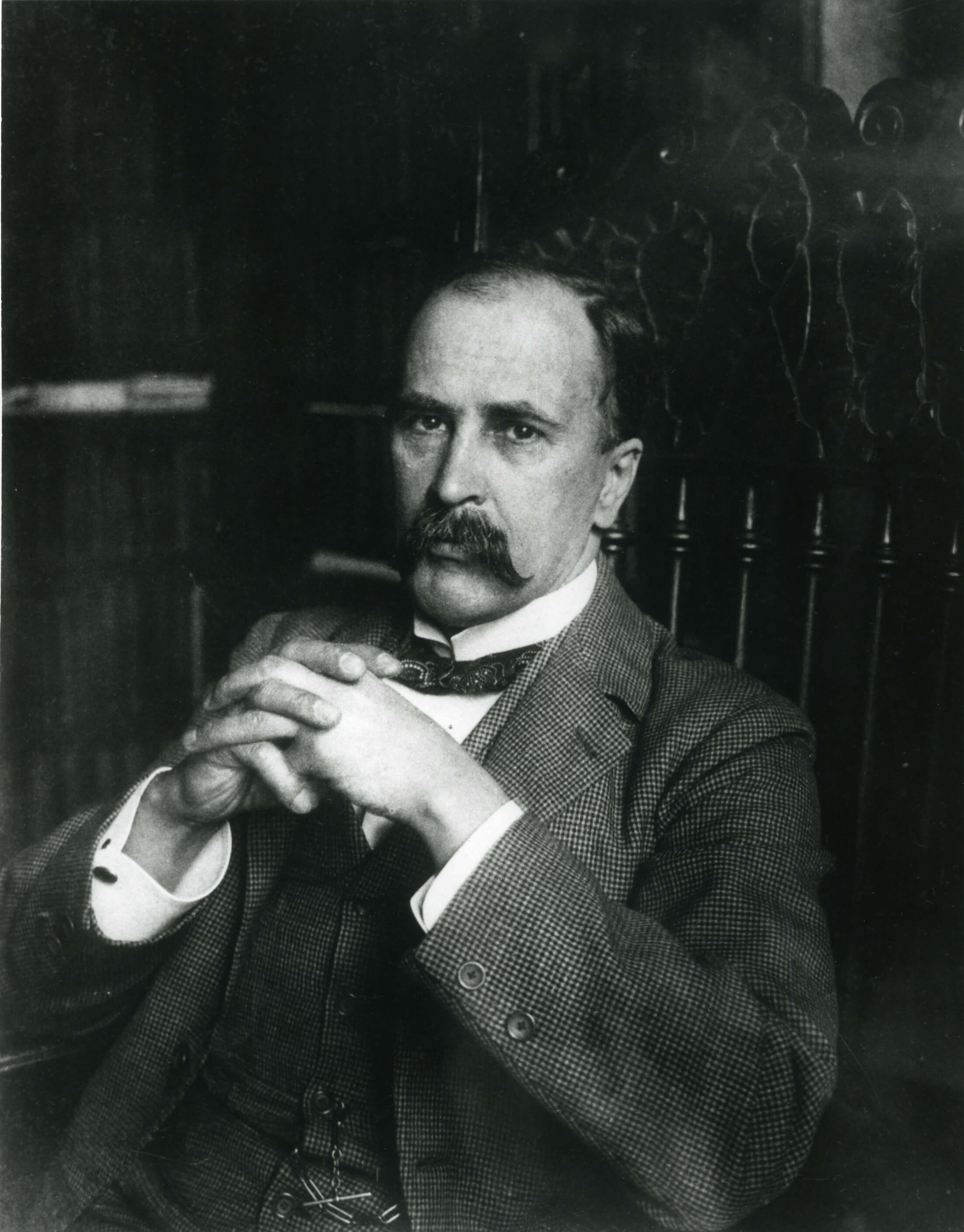 Sir William Osler
Sir William OslerFew individuals had greater influence on American medicine than Osler. Soon after arriving in Baltimore, Osler began making dramatic, progressive changes in medical education. Until that point, medical school consisted of basic science classes and didactic lectures where professors examined patients in large amphitheaters while students observed from above. Osler considered bedside teaching a critical aspect of training new physicians, and this remains a core component of our training program to this day.
Osler also established the full-time, sleep-in residency system whereby staff physicians lived in the administration building of the hospital. The training was open-ended; residents spent as long as seven or eight years in the residency. The contribution to medical education that Osler was most proud of was his idea of clinical clerkships--having medical students work with patients on the wards. He pioneered the practice of bedside teaching, and would make rounds with students and demonstrating what one student referred to as his method of "incomparably thorough physical examination."
Each of the chairpersons who have followed Dr. Osler have helped the department flourish not only by responding to the challenges of the times, but also by adhering to the Oslerian principles of the primacy of the patient and the importance of patient-based education. The department is currently led by Interim Director Dr. Nadia Hansel.
History of The Johns Hopkins Hospital
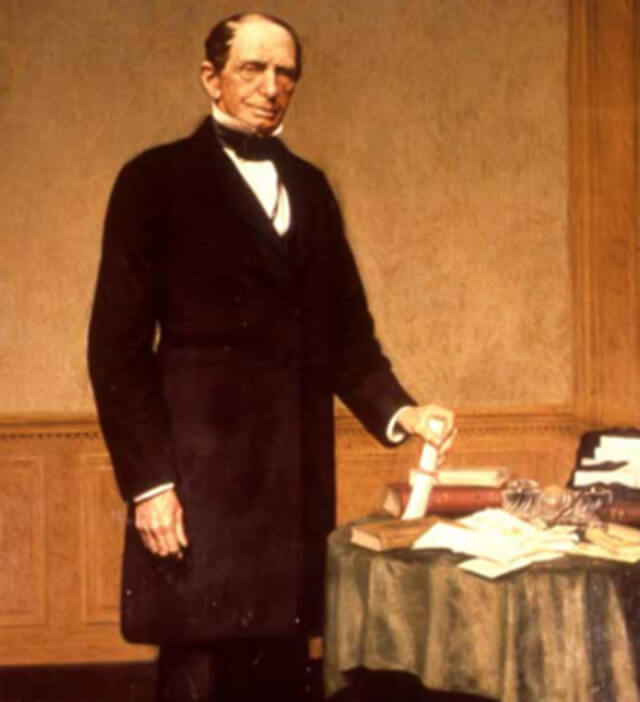 Johns Hopkins
Johns Hopkins
Johns Hopkins, a famous Baltimore businessman, left his fortune of $7 million to establish both the Johns Hopkins University and the Johns Hopkins Hospital. His Quaker upbringing helped him to develop a sense of charity and equity. Mr. Hopkins was not able to receive the education he longed for, so he wanted to provide a university for others. Witnessing the epidemics that ravaged Baltimore caused him to realize the need for a hospital.
As part of his bequest, Johns Hopkins stipulated that a school of medicine accompany the hospital. As such, the School of Medicine was opened in 1893. The Johns Hopkins Hospital was completed in 1889, and from the outset its destiny has been inextricably woven with that of the School of Medicine. This policy was established in a letter from Mr. Hopkins to the first trustees of the hospital. "In all your arrangements in relation to this hospital," he wrote, "you will bear constantly in mind that it is my wish and purpose that the institution shall ultimately form a part of the medical school of that university for which I have made ample provision by my will."
More information on the history of the Johns Hopkins Hospital can be found here.
The Johns Hopkins Hospital Today
 The Johns Hopkins Hospital
The Johns Hopkins Hospital
Today, the hospital complex is a collection of more than a dozen "mini-hospitals" and centers, including six hospitals, four health care and surgery centers, over six ambulatory surgery centers, and 50+ primary and specialty care outpatient sites. The hospital offers over 226 separate clinical services and more than 1,000 beds.
The hospital, along with its sister institutions, welcomes an estimated 10,000 visitors and employees each day. The hospital annually provides services for nearly 43,000 inpatient visits, approximately 518,000 outpatient visits, and over 94,000 emergency department visits. More information about the Johns Hopkins Hospital is found here.
