-
Courtenay Mynnette Holscher, M.D., Ph.D.
Expertise: Abdominal Aortic Aneurysm (AAA), Aortic Aneurysms, Carotid Artery Disease, Claudication, Diabetic Foot Care
-
Ying Wei Lum, M.D., M.P.H.

Expertise: Abdominal Aortic Aneurysm (AAA), Aneurysms, Angiography, Angioplasty, Aortic Stent-Grafts/Endografts
-
Joseph Michael White, M.D., M.S.

Expertise: Aneurysm Repair, Angioplasty, Aortic Aneurysms, Carotid Endarterectomy, Complex and Re-operative Vascular Surgery
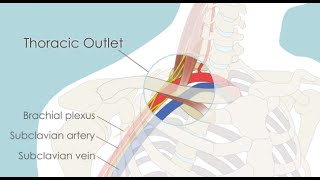
Thoracic Outlet Syndrome Clinic
The Johns Hopkins Thoracic Outlet Syndrome Clinic diagnoses and treats all forms of thoracic outlet syndrome (TOS), whether it is neurogenic (nerve compression) or vascular (blood vessel compression). Our experts study your medical history, run tests to rule out similar conditions, and examine you to develop a clear picture of what’s causing your arm and shoulder symptoms.
-
Our Specialists
Meet the experts who diagnose and treat thoracic outlet syndrome.
-
What You Need to Know
Learn more about symptoms, treatments and prevention.
-
Patient Information
Learn about what to expect, from your first visit to your last treatment.
-
Clinic Locations
View our Baltimore clinic locations.
What is Thoracic Outlet Syndrome; How is it Diagnosed and Treated?
Assistant Professor of Surgery Dr. Ying Wei Lum discusses causes, symptoms and risk factors of thoracic outlet syndrome.
Patient Information: What to Expect
Personalized Treatment
Treatment for thoracic outlet syndrome (TOS) is highly specific to each patient. Expert diagnosis is essential to determine whether nerves or blood vessels are being compressed and which bones or muscles are involved in the compression. If possible, a conservative treatment is often recommended at first — particularly for neurogenic TOS — progressing to injections or surgery only if you don’t find permanent relief with conservative measures.
What to Expect from Your First Visit
Your care team will begin by conducting the following:
- Complete medical history
- Physical examination
- Discussion of symptoms
Thoracic outlet syndrome can sometimes be caused by weight gain, increased muscle mass, injury or repetitive overhead motion. To better understand what might be causing your symptoms, your care team may also ask about:
- Work and lifestyle activities
- Recent injuries or changes
Appropriate diagnostic scans may then be performed.
What to Expect from Your Treatment
A customized treatment plan will be developed by your care team based on your type of TOS, the severity of your condition, and previous treatments you have received. TOS treatments include:
-
The first-line treatment for neurogenic TOS, the most common type, is physical therapy. Often it’s the only treatment many patients will need. We provide a set of written instructions you can bring to a physical therapist, or you can visit the Johns Hopkins Medicine Department of Physical Medicine and Rehabilitation.
Length of treatment: The normal course of treatment is six to 10 weeks, with two to three sessions per week. If physical therapy does not provide relief, you can return to the clinic for further treatment.
Resuming activity: You will be taught how to do “maintenance” home physical therapy exercises on your own to manage your shoulder if your symptoms are controlled during the formal physical therapy sessions. Most patients are able to resume their normal activities if physical therapy is successful.
-
If physical therapy doesn’t relieve your symptoms, further diagnostic tests, such as an initial injection of local anesthetic into the scalene muscles, may be recommended. If you respond to this diagnostic injection, then botulinum toxin may be helpful.
In this treatment, a small amount of botulinum toxin is injected into the scalene muscles near the site where they are thought to be compressing the nerves.
Length of treatment: In rare cases, a single-dose injection may give permanent relief. However, most treatments usually last two to three months.
-
There are several different approaches to decompression surgery. Your vascular surgeon will opt for the one that best treats your condition.
Length of stay: Depending on the type of TOS and kind of surgery that is performed, most patients stay in the hospital for one day and are ready for discharge from the hospital the day after surgery. If you’re coming from out of town, you should expect to stay in Baltimore for two to three days before returning home.
Recovery: Most patients will feel some level of discomfort/pain as they recover from surgery for at least 1-2 weeks.
Return to activity: Patients often to return to light activity in seven to 10 days. Returning to work, therefore, will depend on the physical demands of the job. We strongly recommended you not overexert yourself by doing any repetitive overhead movements or lifting more than 10 to 15 pounds for three months.
Physical therapy: The course of physical therapy begins two weeks after surgery. We recommend you attend two to three sessions per week, for eight to 12 weeks. You can visit a physical therapy practice that is convenient for you. You will be given specific written physical therapy instructions to provide to your therapist.
-
Lemore Carmi, M.D.

Expertise: Chronic Total Occlusions, Claudication, Diagnostic Radiology, Lower Extremity Angioplasty, Lower Extremity Stenting
-
Paul Jordan Christo, M.D.

Expertise: Anesthesiology, Back Pain, Complex Regional Pain Syndrome, Diminished Ovarian Reserve, Disc Pain
-
Brian Philip Holly, M.D.
Expertise: Abnormal Uterine Bleeding, Angiography, Angioplasty, Arteriovenous Fistulas (AVF), Arteriovenous Malformations (AVM)
Clinic Staff
Asma Abeer, M.S., PA-C
Physician Assistant
Asma Abeer received her Bachelor of Science in Biology and minor in Gerontology at Ramapo College of New Jersey. She then went on to obtain her Master of Science in Physician Assistant Studies from DeSales University. Following graduation, Asma joined the Division of Vascular Surgery at Johns Hopkins Bayview and has worked there since. Asma primarily manages peri-operative patients in the outpatient setting and assists with vascular patients in the inpatient setting as well.

Holly Grunebach, P.A.-C., M.S.P.H.
Physician Assistant
Holly Grunebach studied biology and dance at Slippery Rock University in Pennsylvania, then received an MS in physicians’ assistant studies and another MS in public health from Arcadia University. After a year of emergency-room work, Holly entered the Postgraduate Surgical Residency for Physician Assistants program at The Johns Hopkins Hospital. For the last five years, she has worked in the Division of Vascular Surgery. Holly has spent much of that time in the Thoracic Outlet Syndrome Clinic, assisting surgeons in the operating room and at the clinic.

Lindsay Keilholtz
Triage Nurse Lindsay received her bachelor’s degree in nursing at Virginia Commonwealth University (VCU). She began her career at VCU Medical Center as a nurse in the cardiac medical intensive care unit where she worked for two years. Lindsay joined Johns Hopkins in 2009 as a nurse in the cardiovascular surgical intensive care unit where she cared for cardiac surgery patients, trained new nurses in the ICU and served as a clinical resource nurse for younger staff. In 2015, Lindsay became the second triage nurse for the Department of Surgery, working with the cardiac and vascular surgery teams. She also serves as the first point of contact for all new cardiac and vascular patients admitted to Johns Hopkins Heart and Vascular Institute.

Our Locations
Johns Hopkins Bayview Medical Center
4940 Eastern Ave
Baltimore, MD 21224

The Johns Hopkins Hospital
1800 Orleans St
Baltimore, MD 21287

Suburban Hospital
8600 Old Georgetown Rd,
Bethesda, MD 20814

Surgical Treatment for Thoracic Outlet Syndrome | Mark’s Story
When Mark Norwich was determined to find a treatment for thoracic outlet syndrome that would allow him to start in his college football program. The Norwich family traveled from New York City to Baltimore to see Dr. Ying Wei Lum. Mark and his family tell the story of the surgical treatment, rehabilitation and recovery from thoracic outlet syndrome.
Treatment for Thoracic Outlet Syndrome | Aaron's Story
Aaron Hoover first felt the shoulder pain while pitching in a college baseball game. After numerous tests and scans, Aaron's doctor found a blood clot — a major clue that he had Thoracic Outlet Syndrome. Aaron talks about his experience with the Johns Hopkins Thoracic Outlet Syndrome clinic, from surgery to recovery.
Transaxillary First Rib Resection for Thoracic Outlet Syndrome (TOS)
Learn more about the tranaxillary first rib resection surgical approach to treat TOS from the Johns Hopkins Thoracic Outlet Syndrome Clinic. Watch to find out what happens during and after this decompression surgery, which is a low risk and effective surgical treatment for patients diagnosed with neurogenic or venous TOS.
Nerve Block Treatment for Thoracic Outlet Syndrome (TOS)
Nerve Block is a non-surgical alternative for patients suffering from Thoracic Outlet Syndrome (TOS). This animation illustrates how physicians at the Johns Hopkins Thoracic Outlet Syndrome Clinic perform interscalene brachial plexus blocks using botulinum toxin type A injections to provide temporary pain relief for patients.
Read about our treatment approaches:
- Read more about TOS and how Ying Wei Lum, M.D. has become the go-to doctor for the unusual condition
- Learn more about the signs, symptoms and diagnosis of thoracic outlet syndrome
- Take a look at how far our patients travel for treatment of thoracic outlet syndrome
- Thoracic Outlet Syndrome Diagnosis and Treatment: A Johns Hopkins Mainstay