Patient Story
Mitral Valve Replacement: Waveney’s Story

Patient Story Highlights
- At 54, Waveney Springer began experiencing debilitating chest pains that came on without warning.
- Surgeon Thomas Matthew diagnosed her as having a stenotic mitral valve, resulting from rheumatoid fever as a child. He performed a minimally invasive mitral valve replacement in April 2022.
- Waveney is now symptom-free and has more energy than before.
Chest Pains Came on Without Warning
When Waveney Springer started experiencing sudden, intense chest pains, she thought they were caused by stress. The Prince George’s County resident, 54 at the time, was extremely busy running both a hair salon and a natural beauty product business.
The pain began to interfere with her life. She was tired all the time, and struggled to stay on her feet all day at work. She became afraid to drive her car or even go for walks through her neighborhood because she didn’t know when the problem would strike. What if she fainted while driving? Or experienced so much pain during a walk that she couldn’t get home?
“I might just be fine one minute, and the next minute I was having real severe pains in my chest,” she says. “I would be getting dressed to go out, and I’d get such sharp pains that I couldn’t move. Then I wouldn’t go.”
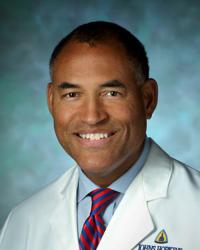
One night, as she was helping her husband clear the dinner table, she stood up and promptly passed out. Waveney’s husband and one of their daughters took her to a local urgent care center, starting a cycle of testing and referrals that eventually led her to Thomas Matthew, M.D., director of the Johns Hopkins Cardiothoracic Surgery Program at Suburban Hospital.
Matthew diagnosed Waveney with a stenotic mitral valve, caused by scarring from rheumatic fever she had suffered as a child. The mitral valve, located between the left atrium and the left ventricle, is one of four valves that pump blood through the heart and out to the body.
With the narrowed mitral valve, Waveney’s heart was less efficient, explaining her weakness, chest pains and dizziness.
A Minimally Invasive Procedure
Matthew recommended a minimally invasive procedure to replace the valve, but first he met with Waveney twice to make sure she was comfortable with his proposal and to create a positive patient-doctor relationship.
Those conversations made an impression on her. “I admired that he thought our relationship was important, that he wanted me to be comfortable,” she says. “It meant a lot. No doctor before has ever told me something like that.”
In April 2022, Matthew performed a mitral valve replacement on Waveney, using a minimally invasive technique. The procedure that he used reduces recovery time and scarring compared with a valve replacement via sternotomy.
A sternotomy opens the chest by dividing the sternum from the top to the bottom of the breast bone, an intervention that typically requires a six- to eight-week recovery. The minimally invasive procedure, by contrast, uses a small incision of about 3 inches at the breast, requiring a recovery of about two weeks.
Matthew and fellow cardiac surgeon, Reed Quinn, M.D., also perform valve replacements using sternotomies when necessary, often because other procedures are done at the same time, such as a coronary bypass.
Both procedures require anesthesia and a heart-lung bypass machine, but with the minimally invasive option, surgeons access the valve through a small incision at the breast and between the ribs to remove the damaged valve, then suture the ring around the mitral valve, called the annulus, and bring the sutures through the new valve before closing the incision.
“The procedure is the same, but it’s a much smaller access point, which makes for a faster recovery,” says Matthew.
A year later, Waveney says her symptoms are gone, and she feels more energetic than she has in a long time. The only medication she takes is a blood thinner to prevent clots, and she hasn’t noticed any side effects from it.
No More Living in Fear
The best thing, says Waveney, who has three children, is that she is no longer afraid that she’ll double over in pain or faint without warning. She’s able to devote her newfound energy to her businesses, her family and to herself.
“It used to be that I couldn’t walk in the cold,” she says. “I couldn’t catch my breath. Now I can go out and walk. I was out this morning and it was cold, and I’m good. It’s a huge relief.”
Waveney's Cardiac Surgeon
Cardiothoracic Surgery at Suburban Hospital
The Johns Hopkins Cardiothoracic Surgery Program at Suburban Hospital, led by Thomas Matthew, offers state-of-the-art surgical treatments, including valve replacements and repairs. Learn more about cardiac services at Suburban Hospital.