Mitral Valve Replacement
What is a mitral valve replacement?
A mitral valve replacement is a surgery to replace a poorly working mitral valve with an artificial valve. The mitral valve is 1 of the heart’s 4 valves. It helps blood flow through the heart and out to the body. The mitral valve lies between the left atrium and the left ventricle. Your doctor will replace your poorly working mitral valve with an artificial valve. This will ensure that blood can flow into the left ventricle and then flow out to the body normally, without putting extra stress on the heart. The surgery this article focuses on uses a traditional larger incision to expose the heart. This incision is larger than the incision used in minimally invasive mitral valve replacement surgery.
Frequently Asked Questions About the Mitral Valve
Why might I need a mitral valve replacement?
The procedure may be necessary if the mitral valve is working poorly. Surgical repair of the mitral valve is often possible, but sometimes the valve needs to be replaced.
Mitral valve stenosis and mitral valve regurgitation (also known as mitral insufficiency) are two different types of problems that might need valve replacement.
- In mitral valve stenosis, the valve is unable to open fully, and less blood is able to move from the left atria into the left ventricle.
- In mitral valve regurgitation, the valve is leaky. Some blood leaks back into the left atrium instead of moving forward into the left ventricle.
These valve problems can lead to such symptoms as fatigue and shortness of breath. If these symptoms become severe, surgery may be necessary.
Both mitral stenosis and mitral regurgitation can result from general aging of the valve. Other causes of mitral valve disease include:
- Ischemic heart disease (coronary artery disease)
- Infection of the heart valves
- Heart failure
- Rheumatic fever
What are the risks of a mitral valve replacement?
Most people who have a mitral valve replacement have a successful outcome, but there are certain risks. Your particular risks will vary based on your overall health, your age and other factors. Be sure to talk with your doctor about any concerns that you have. Possible risks include:
- Infection
- Bleeding
- Irregular heart rhythms
- Blood clots leading to stroke or heart attack
- Complications from anesthesia
- Continued leaking of the valve
- Damage to nearby organs
- Memory loss or problems with concentration
Certain factors increase the risk of complications, like:
- Chronic illness
- Other heart conditions
- Lung problems
- Increased age
- Being obese
- Being a smoker
- Infections
How do I get ready for a mitral valve replacement?
As you plan for the surgery, you and your doctor will decide what kind of valve will work best for you. Your surgeon will replace your valve with a biological valve or a mechanical valve.
- Biological valves are made mainly from pig, cow or human heart tissue. Biological valves don’t last as long as mechanical valves
- Mechanical valves are man-made. If you receive a mechanical valve, you will need to take blood-thinning medicine for the rest of your life. Mechanical valves also have an increased risk of infection.
Talk with your doctor about how to prepare for your upcoming surgery. Remember the following:
- Avoid eating or drinking anything after midnight before your surgery.
- Try to stop smoking before your operation. Ask your doctor for ways to help.
- You may need to stop taking certain medicines before your surgery. Follow your doctor’s instructions if you usually take blood-thinning medicines like warfarin or aspirin.
You may need to arrive at the hospital the afternoon before your operation. This is a good time to ask any questions you have about the procedure. You may need some routine tests before the procedure to assess your health before surgery. These may include:
- Chest X-ray
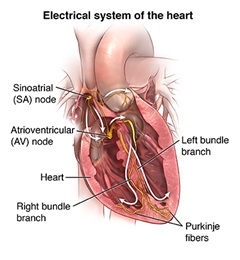
- Electrocardiogram (ECG)
- Blood tests
- Echocardiogram
- Coronary angiogram (to assess blood flow in your heart arteries)
About an hour before the operation, someone will give you medicines to help you relax. In most cases your surgery will proceed as planned, but sometimes another emergency might delay your operation.
What happens during a mitral valve replacement?
Check with your doctor about the details of your procedure. In general, during your mitral valve replacement:
- A doctor will give you anesthesia before the surgery starts. This will cause you to sleep deeply and you will not feel pain during the operation. Afterward you won’t remember it.
- The operation will take several hours. Family and friends should stay in the waiting room, so the surgeon can update them.
- Your doctor will make an incision down the middle of your chest. To access your heart, your doctor will separate your breastbone.
- The surgery team will attach you to a heart-lung machine. This machine will act as your heart and lungs during the procedure.
- Your surgeon will remove your current mitral heart valve and replace it with a new valve.
- The surgery team will remove the heart-lung machine.
- The team will wire your breastbone back together.
- The team will then sew or staple the incision in your skin back together.
What happens after a mitral valve replacement?
After your mitral valve replacement:
- You will begin your recovery in the intensive care unit or a recovery room.
- When you wake up, you might feel confused at first. You might wake up a couple of hours after the surgery, or a little later.
- Most people who have mitral valve replacement notice immediate symptom relief after their surgery.
- The team will carefully monitor your vital signs, such as your heart rate. They may hook you up to several machines so the nurses can check these more easily.
- You may have a tube in your throat to help you breathe. This may be uncomfortable, and you won’t be able to talk. Someone will usually remove the tube within 24 hours.
- You may have a chest tube to drain excess fluid from your chest.
- Bandages will cover your incision. These can usually come off within a couple of days.
- You will feel some soreness, but you shouldn’t feel severe pain. If you need it, you can ask for pain medicine.
- In a day or two, you should be able to sit in a chair and walk with help.
- You may perform breathing therapy to help remove fluids that collect in your lungs during surgery.
- You will probably be able to drink the day after surgery. You can have regular foods as soon as you can tolerate them.
- You may receive elastic stockings to help blood circulate through your leg veins.
- You will probably need to stay in the hospital for around five days.
After you leave the hospital:
- Make sure you have someone to drive you home from the hospital. You will also need some help at home for a while.
- You will probably have your stitches or staples removed in a follow-up appointment in seven to 10 days. Be sure to keep all follow-up appointments.
- You may tire easily after the surgery, but you will gradually start to recover your strength. It may take several weeks to fully recover from your surgery.
- After you go home, take your temperature and your weight every day. Tell your doctor if your temperature is over 100.4°F (38˚C), or if your weight changes.
- Ask your doctor when it is safe for you to drive.
- Avoid lifting anything heavy for several weeks. Ask your doctor about what is safe for you to lift.
- Follow all the instructions your health-care provider gives you for medications, exercise, diet and wound care.
- Make sure all your dentists and doctors know about your medical history. You may need to take antibiotics before certain medical and dental procedures to prevent getting an infection on your replacement valve.
Next Steps
Before you agree to the test or the procedure, make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure
New Co-Director Appointed to the Johns Hopkins Heart and Vascular Institute
James Gammie, M.D., has joined the Johns Hopkins Heart and Vascular Institute as a co-director and surgical lead. Dr. Gammie is an expert in mitral valve repair and performs over 200 procedures each year. He is also an entrepreneur who has launched four companies, and he brings that enthusiasm and spirit of innovation to Johns Hopkins.