Barrett's Esophagus Treatment
Doctors at Johns Hopkins are at the forefront of diagnosing and treating Barrett's esophagus. In fact, gastroenterologists at Hopkins pioneered the use of cryoablation, a revolutionary new therapy, to treat Barrett's esophagus.
Cryoablation involves freezing the Barrett’s esophagus cells to purposefully injure them and stimulate regeneration of normal tissue. Other endoscopic treatments for Barrett’s esophagus are also offered at Johns Hopkins, including endoscopic mucosal resection, radiofrequency ablation, argon plasma coagulation (a noncontact laser) and photodynamic therapy. When you choose Johns Hopkins for your health care needs, you know you are receiving the best care from top experts in the field.
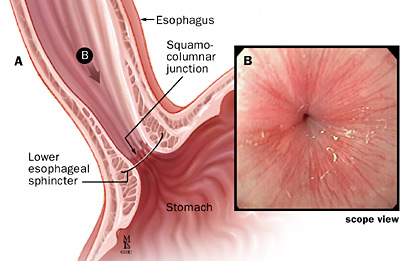
Barrett's esophagus is a complication of reflux disease, in which acid leaking back from the stomach begins to erode the esophagus. The treatment for Barrett's esophagus is similar to the treatment for GERD.
- Lifestyle and dietary changes
- Medication
- Surgery
- Endoscopic therapy
- Cryoablation therapy
- Endoscopic surveillance
Lifestyle and Dietary Changes
Dietary and lifestyle changes are the first steps in treating Barrett's esophagus. Certain foods make the reflux worse. Suggestions to help alleviate symptoms include:
- Avoiding foods that increase the level of acid in your stomach, including caffeinated beverages
- Avoiding foods that decrease the pressure in the lower esophagus, such as fatty foods, alcohol and peppermint
- Avoiding foods that affect peristalsis (the muscle movements in your digestive tract), such as coffee, alcohol and acidic liquids
- Avoiding foods that slow gastric emptying, including fatty foods
- Avoiding large meals
- Quitting smoking
- Remaining upright immediately after a meal
- Elevating your head
- Losing weight (if you are overweight)
Medication
If lifestyle and dietary changes do not work, medications may be prescribed. There are two categories of medicines for reflux. One decreases the level of acid in your stomach, and one increases the level of motility (movement) in the upper gastrointestinal tract.
Antacids
Over-the-counter antacids are best for intermittent and relatively infrequent symptoms of reflux. When taken frequently, antacids may worsen the problem. They leave the stomach quickly, and your stomach actually increases acid production as a result.
Histamine Blockers
Histamine 2 (H2) blockers are drugs that help lower acid secretion. H2 blockers heal esophageal erosions in about 50 percent of patients.
Proton Pump Inhibitors
Proton pump inhibitors (PPIs) are drugs that block the three major pathways for acid production. PPIs suppress acid production much more effectively than H2 blockers. PPIs are the most effective medication for healing erosive esophagitis and providing long-term control of GERD symptoms.
Prokinetic Agents
Prokinetic agents are drugs that enhance the activity of the smooth muscle of your gastrointestinal tract. These drugs are somewhat less effective than PPIs. These may be prescribed in combination with an acid-suppressing drug.
Barrett's Esophagus (Esophageal Cancer) | Tom's Story
Tom Holste learned he had Barrett's Esophagus (esophageal cancer) after suffering from severe acid reflux and heartburn for more than a decade. He went through multiple treatments for his Barrett's Esophagus but it wasn't until he met Marcia Canto, M.D., Director of Clinical Research, Division of Gastroenterology, at Johns Hopkins Medicine that he was cured. Dr. Canto advised a plan to save his esophagus through piecemeal resection and ablation.
Surgery
If you did not find relief from your symptoms from lifestyle changes or drug therapy, then you may be a candidate for surgery. Some patients prefer a surgical approach as an alternative to a lifetime of taking medications. The goal of surgery for reflux disease is to strengthen the anti-reflux barrier.
During a procedure known as a Nissen fundoplication, your surgeon wraps the upper part of your stomach around the lower esophagus. This enhances the anti-reflux barrier and can provide permanent relief for reflux. Your surgeon may perform this surgery laparoscopically, which means the procedure is less invasive and recovery is faster.
Cryoablation Therapy
Gastroenterologists at Johns Hopkins developed the use of cryoablation therapy, an effective treatment for Barrett's esophagus.
Ablation therapy may cause Barrett's esophagus to regress. Medications will be given to suppress your stomach acid. Then, during an endoscopy, thermal injury is administered to the abnormal mucous lining.
Endoscopic Surveillance
Endoscopic surveillance is sometimes recommended. This means that you undergo periodic endoscopic examinations to evaluate whether the condition has evolved into cancer. Your doctor looks for increasing degrees of dysplasia, the abnormal growth of cells, and may perform a biopsy on the area to check for cancerous tissue.
The frequency of your evaluations will depend on the severity of the dysplasia.
- Patients with Barrett's that do not have dysplasia may undergo an evaluation every one to two years.
- Patients with low-grade dysplasia may need an endoscopy every three to six months.
- Patients with high-grade dysplasia may need to undergo an esophagectomy (removal of the esophagus) because of the increased risk of cancer.