Barrett's Esophagus
Barrett's esophagus is a complication of gastroesophageal reflux disease (GERD). GERD is a condition in which the stomach contents, including acid, reflux into the esophagus.
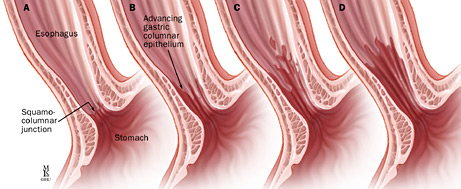
Barrett's esophagus occurs when the lining of the esophagus heals abnormally and changes from cells that look like skin to cells that look like intestinal cells. Hence, Barrett’s esophagus is suspected by the appearance of the esophageal lining (salmon pink color compared to normal white color) and is confirmed by the microscopic examination of cells. It is defined in the United States as intestinal metaplasia.
Who gets Barrett's esophagus?
Roughly 30 million people in North America have GERD. It is the most common chronic gastrointestinal disease. About 5 percent of patients with chronic GERD or inflammation of the esophagus will develop Barrett's esophagus. This condition is more common in men than in women and more common in Caucasian Americans than in African Americans. The average age at diagnosis is 55 years.
Barrett's Esophagus Symptoms
Barrett's esophagus does not cause symptoms. It may be associated with complications of associated GERD. See a gastroenterologist if you experience any of the following symptoms for more than two weeks:
- Heartburn
- Indigestion
- Blood in vomit or stool
- Difficulty swallowing solid foods
- Nocturnal regurgitation (acidic or bitter liquid coming up to the chest or mouth during the night)
Barrett’s Esophagus Diagnosis
At Johns Hopkins, our experienced doctors use their expertise along with the most advanced imaging technologies to make a careful and accurate diagnosis.
We are one of the few centers in the country using endoscopic confocal microscopy (endomicroscopy), in which a powerful microscope is used to help diagnose a condition during an endoscopy. In vivo real-time examination of the cells during endoscopy can be performed by a small microscopic probe or an endomicroscope mounted on a detailed, high-resolution image that is used to identify abnormalities, allowing physicians to detect cancer cells without a biopsy. These “smart biopsies” precisely target the abnormal area, so invasive surgery is no longer necessary.
Barrett's Esophagus Diagnostic Procedures
A diagnosis of Barrett's esophagus begins with a comprehensive physical exam during which you describe your symptoms and medical history. Other diagnostic procedures include:
- Upper endoscopy
- Chromoendoscopy
Upper Endoscopy
A gastroenterologist will most likely perform an upper endoscopy with biopsy to help diagnose Barrett's esophagus. During this procedure, the lining of the esophagus is checked for abnormalities. The endomicroscope is often used to analyze the tissue during an endoscopy, avoiding the need for a more invasive biopsy.
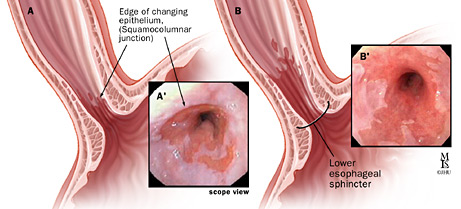
An upper endoscopy allows your doctor to examine the lining of your esophagus, stomach and the first part of your small intestine, called the duodenum. A gastrointestinal endoscopy examines the mucous lining of your upper gastrointestinal tract. The endoscopy and biopsy are two parts of the same procedure:
- Endoscopy refers to the use of a flexible, lighted tube called an endoscope with a camera at the tip. The endoscope is inserted into your stomach through your mouth. There is a camera at the tip of the endoscope so your doctor can see the inside of your body.
- Biopsy means a small tissue sample is removed and sent to a pathology lab for analysis.
During an upper endoscopy:
- You receive an anesthetic to relax your gag reflex. You may also receive pain medication and a sedative.
- You lie on your left side, referred to as the left lateral position.
- Your doctor inserts the endoscope through your mouth and pharynx, into the esophagus.
- The endoscope transmits an image of the esophagus, stomach and duodenum to a monitor that helps your physician guide the endoscope through your esophagus.
- Your physician inserts biopsy forceps into the endoscope to obtain tissue samples.
Chromoendoscopy
A chromoendoscopy also may be used during an upper endoscopy procedure. A chromoendoscopy is a procedure that uses staining to identify abnormal areas that may be malignant (cancerous). During the endoscopy, we apply stains to the esophagus with a liquid called Lugol's solution. The dye stains only the normal cells; unstained areas may be malignant. The unstained areas are easily seen and tissue is removed from that area and sent for biopsy.
Barrett's Esophagus (Esophageal Cancer) | Tom's Story
Tom Holste learned he had Barrett's Esophagus (esophageal cancer) after suffering from severe acid reflux and heartburn for more than a decade. He went through multiple treatments for his Barrett's Esophagus but it wasn't until he met Marcia Canto, M.D., Director of Clinical Research, Division of Gastroenterology, at Johns Hopkins Medicine that he was cured. Dr. Canto advised a plan to save his esophagus through piecemeal resection and ablation.
Barrett's Esophagus Treatment
Barrett's esophagus is a complication of GERD, so your treatment may be similar. The goal is to heal the erosions of the esophageal lining and prevent the condition from spreading. We may use endoscopic surveillance to keep an eye on the progression of the disease. There is a risk of Barrett's esophagus becoming cancerous, so your condition may need to be monitored frequently. If there are precancerous cells (dysplasia) diagnosed in the Barrett’s esophagus, endoscopic treatment is recommended and proven safe and effective for preventing progression to cancer.







