Vulvar Cancer
Reviewed By:
Cancer that forms on the outer surface of the vulva is called vulvar cancer. It is a rare condition — only about 6,400 new cases are diagnosed in the United States each year.
What You Need to Know
- Vulvar cancer is very rare, accounting for 0.7 percent of all cancers in women.
- The HPV vaccine can prevent the strains of HPV responsible for most cervical, vaginal and vulvar cancers.
- Risk factors that may increase a woman’s chances of developing vulvar cancer include age, infection with certain types of HPV, smoking and HIV infection.
- Symptoms of vulvar cancer include severe itching, burning and pain on the vulva.
Vulvar cancer occurs when abnormal cells form and grow in the vulvar tissues. These tissues are part of the vulva, which includes several parts of female genitalia:
- Inner and outer lips of the vagina (labia majora and labia minora)
- Clitoris
- Tissue around the opening of the vagina
- Urethra (this is where urine comes out)
Types of Vulvar Cancer
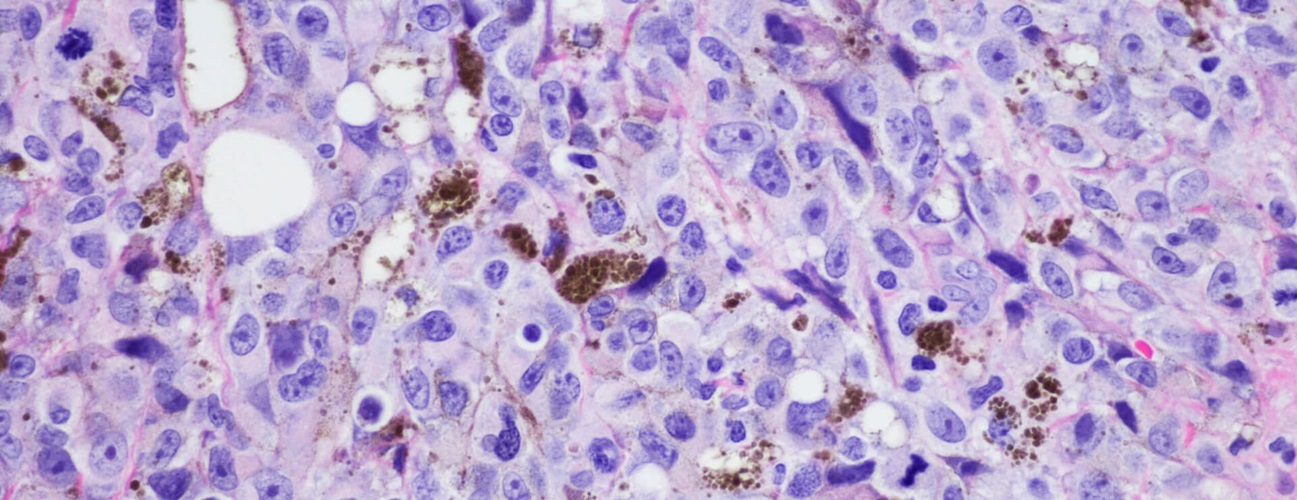
Vulvar cancers are most common in the labia majora and labia minora. Most vulva cancers are squamous cell carcinomas, a type of cancer that starts in the skin cells. Vulvar squamous cell carcinomas form when the thin, flat cells lining the surface of the vagina change (mutate). The mutated cells can multiply quickly.
The following are other, less common types of vulvar cancer.
- Melanoma: The second-most common type of vulvar cancer typically presents as a pigmented lesion on the vulva. Amelanotic lesions can also occur.
- Basal cell carcinoma: This accounts for 2% to 7% of vulvar cancers.
- Bartholin gland carcinoma: Up to 5% of vulvar cancers originate from the Bartholin gland, which is a small gland just inside the vagina opening.
- Sarcoma: This accounts for 1% to 2% of vulvar cancers. These soft-tissue sarcomas include leiomyosarcomas, rhabdomyosarcomas, liposarcomas, angiosarcomas, neurofibrosarcomas, epithelioid sarcomas and undifferentiated/unclassified sarcomas.
- Paget’s disease of the vulva: This accounts for less than 1% of vulvar cancers.
Vulvar Cancer Causes and Risk Factors
Most cases of vulvar squamous cell carcinoma result from two common risk factors — human papillomavirus (HPV) and chronic inflammation or autoimmune processes.
- Human papillomavirus: About half of vulvar squamous cell carcinoma cases are caused by exposure to HPV, which is the most common sexually transmitted infection (STI) in the United States — 43 million people are infected each year. Most people who have the virus are exposed to it by their early 20s, but cancer may develop years after exposure. There is a safe and effective vaccine to reduce the risk of cancer from HPV. The HPV vaccine is for people ages 9 to 45, but it is ideal to receive the vaccine as close to age 9 as possible. HPV infection can lead to precancerous and cancerous vulvar lesions.
- Chronic inflammatory or autoimmune processes: Skin conditions such as lichen sclerosus can lead to development of precancerous and cancerous vulvar lesions that are unrelated to HPV infection.
Other risk factors can also increase a person’s chance of developing vulvar cancer, including:
- Age: About 80% of vulvar cancer is diagnosed in females over the age of 50.
- HIV infection: Human immunodeficiency virus (HIV), which causes AIDS, damages the immune system. This increases the risk of getting HPV and may also affect the body’s ability to find and destroy cancer cells before they spread.
- Lichen sclerosus: This condition causes skin around the vulva to become irritated, thin and itchy. Only about 4% of women with this condition eventually develop vulvar cancer.
- Melanoma: A family history of melanoma or several atypical moles increases the risk of vulvar cancer.
- Other genital cancers: Having other cancers in the genitals, most commonly cervical cancer, can increase the chance of developing vulvar cancer.
- Smoking: Smoking increases the risk of vulvar cancer. The risk is even greater for people with HPV who also smoke.
Having any risk factor — or even more than one — does not mean you will develop vulvar cancer, but it makes vulvar cancer more likely. This is why regular checkups and pelvic exams are important. Your doctor can look for early signs of vulvar cancer during these exams.
Obesity and Cancer Risk

Did you know that up to one-third of cancer deaths in women are attributed to excess body weight? Director of Gynecologic Oncology Amanda Fader and oncology dietitian Mary-Eve Brown discuss the correlation between the two. Learn what you can do to reduce your risk.
Vulvar Cancer Symptoms
The signs of vulvar cancer vary depending on the type of cancer and where it starts. The most common form of vulvar cancer, squamous cell carcinoma, usually has noticeable symptoms, including:
- An open sore that does not heal for several weeks or months
- Bleeding or discharge that is not part of a normal menstrual period
- Growths that look like cauliflower or genital warts
- Itching or burning sensation
- Noticeable lump or bump with a raw surface that feels rough
- Pain on the outside of the vagina
- Discoloration (skin that is lighter or darker than the skin around it, or that appears more red or pink than usual)
Symptoms of Bartholin gland carcinoma may be different than symptoms of other types of vulvar cancer. You may notice a lump near the opening of your vagina. However, this lump could be a cyst, which is not cancerous.
Vulvar Cancer Diagnosis
The best way to diagnose vulvar cancer is by having regular wellness exams with a primary care doctor or a gynecologist. During these exams, the doctor will look for common signs and symptoms of vulvar cancer and may order tests if something looks suspicious.
- Colposcopy: During a colposcopy, a magnifying device is used to get a better look at the skin cells around the vulva to spot signs of cancer. If an area appears suspicious, a biopsy will be performed.
- Biopsy: The vulva area is numbed and a small sample of tissue is removed and sent to a lab, where a pathologist determines if cancer is present. A biopsy is required to confirm a diagnosis of vulvar cancer.
- Imaging: Imaging tests may be ordered if your doctor thinks your vulvar cancer may have spread to other areas of the body. Tests include CT scans, MRI or positron emission tomography (PET) scans.
Genetic Testing Aids Early Detection

Johns Hopkins researchers are developing new detection methods for gynecologic cancers. Learn more and discover how genetic testing for these cancers is saving lives.
Vulvar Cancer Stages
Doctors use cancer staging to describe whether and how far cancer has spread. This can help them develop the best treatment plan for vulvar cancer.
- Stage 1: The cancer is confined to the vulva.
- Stage 2: Cancer has spread to the lower part of the vagina, the urethra (a small tube that connects to the bladder) or the anus.
- Stage 3: Cancer has spread to the upper urethra, vagina, bladder or rectal mucosa, or to nearby lymph nodes.
- Stage 4: Advanced stage vulvar cancer is fixed to bone and has ulcerated lymph nodes or distant metastases. It may have also spread to distant lymph nodes or other parts of the body.
Vulvar Cancer Treatment
The following are among the most common treatments for vulvar cancer.
- Surgery: This is done to remove the lesion from the vulva. It can include a simple, wide local excision or removal of a larger portion of the vulva, depending on the lesion’s location and size. The surgeon also takes out some healthy cells around the cancer to help be sure that all of the cancerous cells are removed.
- Lymph node biopsy: It is important to determine if the cancer has spread to the lymph nodes. For very early vulvar cancers, lymph node removal is not required, but for any tumor that is bigger than 2 centimeters or that has a depth of invasion greater than 1 millimeter, surgical assessment of lymph nodes either through sentinel lymph node biopsy or complete lymphadenectomy is required.
- Radiation therapy: High-powered energy beams are directed at the tumor to kill cancer cells or shrink a tumor before surgery.
- Chemotherapy: Medication kills cancer cells that have spread to other areas of the body. Your oncologist may recommend chemotherapy alone or in combination with radiation and other treatments.
- Immunotherapy: Drugs activate your body’s natural immune system to find and destroy cancer cells.
Vulvar Cancer Prognosis
The prognosis for vulvar cancer varies, depending on how far cancer has spread. Five-year survival rates for vulvar cancer are:
- 86% when cancer is only in the vulva and it has not spread to lymph nodes or local (nearby) tissues
- 53% when cancer cells have spread to nearby lymph nodes, but not to other parts of the body
- 19% when the cancer has spread (metastasized) to distant organs or lymph nodes