Patient Story
Bladder Cancer: Susan’s Story
Four years after completing treatment for bladder cancer at the Johns Hopkins Kimmel Cancer Center at Sibley Memorial Hospital, retired middle school teacher Susan Baltic says she feels like a walking miracle. She’s now living life to the fullest, knowing her urologic surgeon Dr. Armine Smith, who she calls her “super hero,” always has her back.
In early 2016, Susan recognized something was wrong. She found she had to go to the bathroom more and more frequently, which was difficult while teaching. She knew she should see a doctor, but she was working long hours helping design sets for the school play, and figured she’d deal with it over the summer.
A couple of months later, the problem intensified. Sometimes, she needed a bathroom as often as every 10 to 20 minutes, and it got to the point where she knew which stores she frequented or passed by had bathrooms located in the front, so she could get to them quickly.
The final straw was a trip to her son’s house just 26 miles away, when she needed to stop three times to go to the bathroom on the way, and still needed to go again when she arrived. This time, she noticed blood in her urine. “I came out of the bathroom and announced to my son, my daughter-in-law and my husband, ‘You need to hold me accountable. I need to make a phone call first thing Monday morning and make an appointment.”
Initial tests revealed she had an aggressive cancer. Because Susan’s cancer had spread deep into the bladder wall, she would need chemotherapy treatments prior to bladder removal surgery. Dr. Smith went over all of the possible surgical options for Baltic and even suggested other patients she could call to ask questions.
A woman of faith, Baltic prayed about it and chose to have a neobladder if possible—a bladder created from a piece of intestine. Dr. Smith said she would do her best but may have to find another option if she found cancer in the urethra during surgery. She also introduced Baltic to specialized stoma nurses at Sibley who care for bladder and bowel cancer patients, before her procedure.
"Every experience at that hospital was wonderful," Susan says, "from the cystoscopy I had there, the treatments, Dr. Smith, her nurse Laura Eitel, and everyone else. When you're diagnosed with cancer, it's devastating and you're going through new territory that in the back of your mind you just never know what to expect. Everything went smoothly."
Susan underwent surgery on Feb. 2, 2017, which was Groundhog Day. This had particular meaning for her because she had completed her student teaching years ago in Punxsutawney, Pa.—the town known for its annual weather prediction by groundhog Punxsutawney Phil.
Dr. Smith was indeed able to perform the neobladder procedure. However, during her postsurgical visit with Dr. Smith, Susan learned that cancer had been found in a number of lymph nodes, indicating a possibility it could recur. “Now what?” Susan thought.
Dr. Smith replied, “Now you’re going to live stress-free, and we’re going to be on top of it.”
"The diagnosis of cancer is a very stressful one, and many patients with genitourinary cancers develop mood disorders during and after treatment," Dr. Smith says, "I always give this message to them: Let me worry about you so you don't have to. I think it helps."
Aside from periodic imaging scans to monitor for any cancer recurrence, Susan stays busy painting and spending time with her grandchildren. Before the COVID-19 pandemic, she was able to take two dream trips to Africa and to Montana to ride horses. “I take advantage of every opportunity of everything that I can physically do and afford to do,” she says. “I encourage anyone who is having symptoms to not delay in seeking medical attention like I did. An earlier diagnosis may possibly have contained the cancer within my bladder.”
Many patients fear what life will be like after this type of surgery, Dr. Smith says: “Ms. Baltic’s story is an example that it is still possible to live a normal life after bladder removal. She has a perfectly functioning neobladder, which is a composite of the surgeon’s effort and skill and the patient’s vigilance in following the instructions on neobladder care.”
Even during the COVID-19 pandemic, it’s essential for women to see a urologist quickly if they spot blood in the urine or other concerning symptoms that may indicate bladder cancers, Dr. Smith says. The medical community has measures in place to keep patients from exposure to COVID-19. Symptoms may otherwise be written off a urinary tract infection, or as something gynecologic-related, she says: “These patients get multiple antibiotics, and sometimes by the time they see a urologist, their cancer is at an advanced stage. I cannot stress enough the importance of timely workup in women who see blood in the urine.”
Susan's Surgeon
Greenberg Bladder Cancer Institute
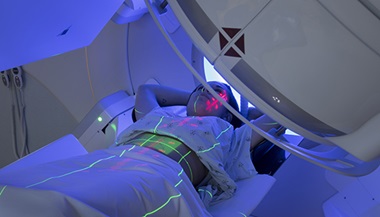
At the Johns Hopkins Greenberg Bladder Cancer Institute, we practice multi-disciplinary care for every single patient. This means that the entire care team — urologic oncologists, medical oncologists, radiation oncologists, radiologists, pathologists and basic scientists — works closely together to make an accurate diagnosis and develop individualized treatment plans.