Innovations in Clinical Care
The Innovations in Clinical Care award is presented to the physician, nurse and/or team who demonstrates a visionary approach to problem solving and performance improvement.
Shahriar Amin, M.D., and the Special Care Unit Patient Care Technicians
Medical Director, Intensive Care and Special Care Units
Johns Hopkins Howard County Medical Center
With guidance from Shahriar Amin, the patient care technicians (PCTs) on the special care unit recently worked together to implement new procedures that will improve and further prioritize patient care and safety. The team evaluated existing processes and determined the best ways to streamline their workflow. The PCTs identified strategies to restock patient rooms more frequently, ensuring that shift change nurses have everything they need during hand off. They also redesigned rounds during the bedside shift change to improve and streamline communication with patients and families. “These are just some of the examples of how the PCTs in the special care unit put their patients first and lead by example,” says a colleague.

Jasmine Reese, M.D., M.P.H. and the Outpatient Eating Disorder Clinic Team
Johns Hopkins All Children’s Hospital
(Team members: Sarah Sobalvarro, Ph.D., Rebekah Diaz, Tacarra Gray, Alexis Dosal, Psy.D., Karen Diaz, Kristen Turner)
The outpatient eating disorder program is an interdisciplinary clinic that brings together specialists in adolescent medicine, psychology, psychiatry, social work, nursing and nutrition. Inpatient eating disorder admissions at Johns Hopkins All Children’s Hospital have increased nearly 200% since the beginning of the COVID-19 pandemic. The outpatient program helps meet the needs of many of these teens and provides early identification and early intervention, reducing the need for hospitalization.
The multidisciplinary clinic draws patients and families from across the region and state. The team evaluates more than 200 teens per year and has helped many patients achieve positive outcomes of recovery, weight restoration and improvement in mental health. The team has used several innovative approaches to treatment and research, including bioimpedance measurements to help assess disease severity and development of individualized treatment plans. The team also developed a novel way to help gauge patient food resistance by routinely offering food items in real time.
To raise awareness about eating disorders and the outpatient clinic, educational sessions were offered for community leaders, medical practitioners, teachers, social workers, athletic trainers, students and parents. The team provides informational resources and strives to make the referral process easy for patients and families to access.

Christopher Lippincott, M.D., and the Center for Nontuberculous Mycobacteria and Bronchiectasis Team
Johns Hopkins Bayview Medical Center
The Johns Hopkins Center for Nontuberculous Mycobacteria (NTM) and Bronchiectasis offers the highest quality of integrated, multidisciplinary care for patients with some of the most challenging infections and underlying conditions. Christopher Lippincott and his team of infectious disease specialists, pulmonologists, clinical pharmacologists and physical therapists typically begin evaluating a patient’s case before the patient reaches the clinic, mentoring referring physicians through treatment and laying the groundwork for what becomes a years-long relationship with the patient.
The center is a magnet for referrals from throughout the health system, including referrals regarding infectious diseases and pulmonology, as well as surgical subspecialties such as plastic surgery and orthopedics. It is also emerging as one of the country’s top referral centers for challenging NTM and bronchiectasis cases. To date, the team has treated patients from 30 states and Washington, D.C.
The Center for NTM and Bronchiectasis team embraces these referrals with enthusiasm through weekly multidisciplinary conferences where they collaborate on complex cases before seeing patients in clinic. The center provides innovative care, and its integrated services make the center a medical home for patient who, for years, have had nowhere else to turn.
Maura McGuire, M.D., Chris Rawlinson, M.S.N., and the MA Externship Program
Johns Hopkins Community Physicians
Maura McGuire, M.D.
Executive Director, Education and Training
Johns Hopkins Community Physicians
Assistant Dean of Part-Time Faculty and Director of the Longitudinal Clerkship
Johns Hopkins University School of Medicine
Chris Rawlinson, M.S.N.
Director, Education and Nursing
Johns Hopkins Community Physicians
Medical Assistant Externship Team
Tara Fisher, Nichole Jantzi, M.S.H.S., Caroline Lentz, M.A., and Trisha Taylor
Johns Hopkins Community Physicians
When Johns Hopkins Community Physicians (JHCP) leadership noted challenges with hiring a sufficient number of certified medical assistants (CMAs), Chris Rawlinson and her team sprang into action. With support and guidance from Maura McGuire, Rawlinson and the team members leveraged new and existing relationships with local CMA training programs to provide externships at JHCP practices. From July 2022 and June 2023, 62 externs were placed, of whom 21 were hired (a 34% conversion-to-hire rate). This filled close to a third of JHCP’s CMA vacancies.
Born out of this externship initiative was a related project that kicked off in fiscal year 2023: a CMA apprentice program. This program allows nonclinical support team members to complete a curriculum qualifying them to become certified as medical assistants. Rawlinson and her team expect to expand both programs to other parts of Johns Hopkins Medicine in fiscal year 2024.

Preeti Raghavan, M.B.B.S., and the Stroke Recovery and Rehabilitation Team
The Johns Hopkins Hospital
In the six years since its inception, the interdisciplinary team at the Johns Hopkins Sheikh Khalifa Center of Excellence in Stroke Treatment, Recovery and Rehabilitation, led by physical medicine and rehabilitation specialist Preeti Raghavan, has blazed trails with novel clinical approaches that have significantly elevated the global standard of stroke care and helped numerous patients receive timely, evidence-based rehabilitation to reduce long-term disability resulting from stroke.
The team’s physicians, physical therapists, occupational therapists, speech and language pathologists, psychologists, rehabilitation engineers and data scientists have integrated stroke care into the inpatient and outpatient rehabilitation continuum as well as into acute care at Johns Hopkins. They’ve implemented a standard battery of measures across the institution for all patients being treated for stroke. And along with the Precision Rehabilitation Center of Excellence, they’ve developed a system to analyze clinical data from electronic medical records that can help build models for precision stroke care.
In February 2023, an entire supplemental issue of the American Journal of Physical Medicine & Rehabilitation was published detailing the lessons the Sheikh Khalifa Center learned in forging a new model of stroke care.
“We’re working on new pathways to help us translate our cutting-edge research into meaningful policy ideas,” says Dr. Raghavan. “Our goals are to become the preeminent source of academic expertise for evidence-based stroke care and to create the leading academic hub for data science and artificial intelligence to drive research and teaching across Johns Hopkins and around the world.”
Brett Parker, M.D., Olaya Brewer Gutierrez, M.B.B.S., and the Gastrointestinal Surgery Team
Sibley Memorial Hospital
- Brett Parker, M.D., general surgeon and fellowship-trained minimally invasive foregut and bariatric surgeon, and program director for the Johns Hopkins advanced GI and minimally invasive surgery fellowship program
- Olaya Brewer Gutierrez, M.B.B.S., director of endoscopy, and assistant professor of medicine, Johns Hopkins University School of Medicine
- Gastrointestinal surgery team
- Mark Andrejkovics, operating room
- Carrie Baumann, gastroenterology clinic
- Arlene Blake, minimally invasive surgery
- Hannah Boyle, operating room
- Joy Bright-Agindotan, gastroenterology
- Tressa Dyson, administrative assistant, endoscopy residents
Brett Parker and Olaya Brewer’s visionary leadership in establishing innovative treatments for gastroesophageal reflux disease (GERD) has significantly impacted the lives of countless patients. They have not only demonstrated exceptional medical expertise but also a deep commitment to pushing the boundaries of traditional treatments with the help of their gastrointestinal surgery team. One of their groundbreaking interventions is the transoral incisionless fundoplication procedure, a minimally invasive approach that has revolutionized GERD treatment by providing an effective alternative to traditional surgical methods. Additionally, the introduction of magnetic sphincter augmentation of the gastroesophageal junction further underscores their dedication to advancing patient care. This novel therapeutic approach has proved highly effective in managing foregut disorders, offering a new frontier in the field. The comprehensive assessments conducted at their center, coupled with these cutting-edge treatments, have collectively elevated the standard of care for people with these challenging conditions.
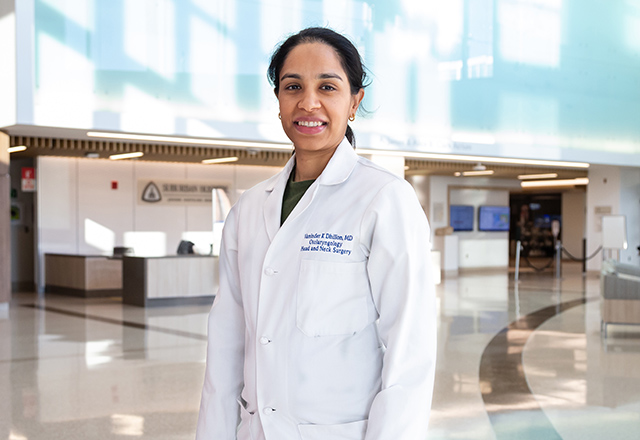
Vaninder Dhillon, M.D., and the Chronic Cough Clinic Team
Otolaryngologist, Johns Hopkins Otolaryngology – Head and Neck Surgery
Suburban Hospital
Chronic cough is a complicated condition, and its treatment can span multiple disciplines. During the past few years, Vaninder Dhillon has pioneered the innovative procedure superior laryngeal nerve block. Dhillon treats hundreds of patients each year with this technique, some of whom travel internationally to see her, and she works with speech language pathology to ensure these patients receive multidisciplinary continuity of care. “Dr. Dhillon has allowed for significant improvement in the quality of life in patients with chronic cough while advancing the field,” a colleague says. “She is recognized among colleagues both within and outside otolaryngology for her expertise, and she has spoken on this treatment in national and international forums. This is an advancement of a clinical innovation beyond the Johns Hopkins Medicine practice.”