Research
Patients with melanoma or other skin cancers seeking care at Johns Hopkins receive the highest standards of care with the latest technologies, mastered by skilled experts in the Johns Hopkins Melanoma/Skin Cancer Program. Importantly, patients have access to emerging therapies that are generated by research discoveries in Johns Hopkins laboratories. Our clinical research program offers studies for patients with both early- and late-stage skin cancers, including melanoma, basal cell carcinoma, cutaneous squamous cell carcinoma and Merkel cell carcinoma. These clinical trials focus on preventing disease recurrence in high-risk surgical patients, as well as developing innovative therapies for patients with advanced metastatic disease.
Our medical and surgical oncologists also collaborate with research partners across the United States and around the world -- including those in academic medical centers, cooperative inter-institutional research groups and pharmaceutical firms -- to conduct clinical trials generating the latest advances in skin cancer therapy. Melanoma/skin cancer research experts at Johns Hopkins are at the forefront of developing the next wave of therapies and diagnostic tools. Ongoing clinical trials are described in more detail in our Clinical Trials section.
Immunotherapy
A main culprit in the development of melanoma and other skin cancers is the ability of cancerous cells to evade the body’s natural defenses against foreign and diseased cells. Johns Hopkins scientists have pioneered ways to educate the immune system to detect, find and destroy skin cancer cells, by arming T lymphocytes with specific capabilities. Our scientists have performed first-of-its-kind research on inhibitory receptors such as PD-1 expressed by immune cells, which bind to molecules such as PD-L1 on melanoma or other kinds of cancer cells and shield them from the immune system. Such interactions restrain anti-tumor immunity, allowing cancer cells to survive and spread. In collaboration with industrial partners, Johns Hopkins scientific and clinical researchers developed effective monoclonal antibody therapies to block these interactions in patients with advanced melanoma (nivolumab, Opdivo), Merkel cell carcinoma (pembrolizumab, Keytruda), and other cancer types, leading the Food and Drug Administration (FDA) to approve such therapies as new standards of care. Such treatments are now also available for patients with advanced basal and squamous cell cancers. These developments have revolutionized our treatment approach to advanced skin cancers. Learn more about this immune system boosting cancer therapy.
Anti-LAG-3: A Novel Immunotherapy for Melanoma
PD-1 and PD-L1 are called “immune checkpoints,” because their interaction with each other blocks the anti-tumor immune response. There are many other immune checkpoints, each with unique properties, that are being studied in our labs and clinics as possible targets for new immunotherapies. One such checkpoint is LAG-3 (lymphocyte activation gene-3). The role of LAG-3 in restraining cancer immunity was discovered by Hopkins scientists over a decade ago. Since then, clinical researchers in the Hopkins Melanoma/Skin Cancer Program have been working with industrial partners to develop LAG-3-blocking antibodies to treat patients with melanoma and other advanced cancers. In March 2022, the FDA approved a combination treatment including anti-PD-1 plus anti-LAG-3 (nivolumab + relatlimab, Opdualag) as the first systemic treatment that a patient with advanced melanoma might receive. A multicenter clinical trial involving several hundred patients confirmed that this combination therapy was significantly more effective in delaying the time to melanoma progression, compared to anti-PD-1 alone (nivolumab, Opdivo). Studies involving melanoma have led the way in testing this new immunotherapy treatment combination against other types of cancer. Read more about immunotherapy for Melanoma.
Harnessing the Immune System to Fight Cancer
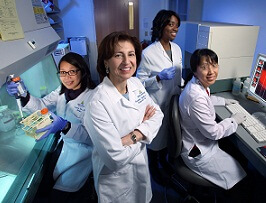
Drs. Suzanne Topalian, Julie Brahmer, Drew Pardoll and lung cancer patient David Gobin discuss anti-PD-1 and anti-PD-L1 therapy in the video “Harnessing the Immune System to Fight Cancer,” produced by Johns Hopkins.
Molecularly Targeted Therapies
BRAF Gene
Approximately 50 percent of melanomas contain a specific mutation in the BRAF gene, which involves a substitution of one of the chemical bases or nucleotides (adenine, thymine, cytosine and guanine) that make up DNA. The order in which these nucleotides occur determines the information that genes communicate to cells for manufacturing new proteins, much like specific letters of the alphabet combine to form words and sentences. In the case of BRAF, a single coding error among more than 2,000 nucleotides in the gene causes the BRAF protein to be stuck in the “on” position, making melanoma cells continuously grow and divide. In collaboration with pharmaceutical companies, Johns Hopkins Melanoma/Skin Cancer Program researchers have evaluated drugs that can block the abnormal signaling caused by the common BRAF driver mutation in patients with advanced metastatic melanoma, leading to FDA approvals for three new treatment regimens combining inhibitors of mutant BRAF and a cooperating molecule, MEK. Johns Hopkins researchers are also developing blood tests to find mutant BRAF DNA shed from dead tumor cells (“liquid biopsy”). Such tests, if successful, may improve diagnostics and detect melanoma growth or recurrence before changes become evident on routine CT or PET scans.
Additional Gene-Targeting Studies
C-Kit is a cancer-promoting gene that is mutated or over-expressed in certain forms of melanoma, including acral and mucosal melanoma. NRAS is another cancer-promoting gene that is mutated in about 20% of cutaneous melanomas. Johns Hopkins researchers are involved in clinical trials designed to test several new drugs directed at these genetic abnormalities found in advanced melanomas.
Prognostic and Predictive Biomarkers
Investigators in our program are leading large multicenter studies to discover markers in tumor biopsies that will provide reliable information on prognosis (natural cancer history, meaning without treatment) or prediction of treatment outcomes with a particular drug. One such study led to the first description of a predictive PD-L1 immunohistochemistry (IHC) marker for successful anti-PD-1 therapy in 2012 . Several commercial PD-L1 IHC tests are currently FDA-approved and in standard use. More complex markers, analyzed with artificial intelligence and machine learning, may provide more sensitive and accurate read-outs and are now in development in our laboratories.
AstroPath
Janis Taube, MD, MsC, explains how AstroPath, an experimental biopsy analysis platform that she developed with Alex Szalay, PhD, of Johns Hopkins University, pairs astronomy with pathology to identify predictive biomarkers for cancer immunotherapy.