Proton Therapy
Proton therapy is an advanced and highly precise radiation treatment for tumors. Compared with other methods, it focuses more energy on the tumor itself with less radiation to surrounding healthy tissue.
What You Need to Know
- Proton therapy is usually painless, and you can often return to your daily activities afterward.
- A typical course of treatment is five days per week for several weeks.
- The proton beam treatment only takes a few minutes, but preparation and positioning take longer.
What is proton therapy?
Proton therapy, also known as proton beam therapy, is a radiation treatment that precisely delivers a beam of protons to disrupt and destroy tumor cells. Compared with traditional radiation, protons have unique properties that allow doctors to better target radiation to the size and shape of the tumor. The proton beam kills the tumor cells and spares more of the surrounding healthy tissue.
What is proton therapy used for?
While proton therapy is most often used to treat cancer, it can also be used to treat noncancerous (benign) tumors in children and adults. Proton beams can be used to treat tumors composed of different types of cells and located in different parts of the body; some examples include:
- Brain tumors, including those in the base of the skull
- Spinal cord tumors
- Head and neck cancer
- Breast cancer
- Lung cancer ;and other ;thoracic cancers such as thymoma, mesothelioma and lymphoma
- Liver cancer and metastatic tumors of the liver
- Pancreatic cancer
- Rectal cancer
- Prostate cancer
- Tumors that come back and need repeat courses of radiation (reirradiation)
- Sarcomas, including rhabdomyosarcoma
- Eye cancer, such as ocular melanoma
Researchers are studying the potential benefits of proton beam therapy on different kinds of cancers.
How Proton Beam Therapy Works
Proton beam therapy works by disrupting the tumor’s DNA and destroying tumor cells. Protons are separated from hydrogen atoms and sped up in a particle accelerator such as a synchrotron or cyclotron. A special device — usually a gantry that can rotate 360 degrees — uses a large magnet to focus the stream of protons into a thin beam, just 5 millimeters wide. The magnet then guides the beam and directs it at the tumor from multiple angles, as the gantry rotates around the patient. The energy within the proton beam can be adjusted based on the depth of the tumor, so that different amounts of radiation can be delivered to different parts of the tumor.
The radiation from protons damages the DNA of the tumor, making the tumor unable to repair itself or grow new cells. This means a tumor stops growing and starts shrinking. The effects of proton radiation vary depending on the size of the tumor, its location and other factors.
Proton Beam Therapy | The Synchrotron Particle Accelerator
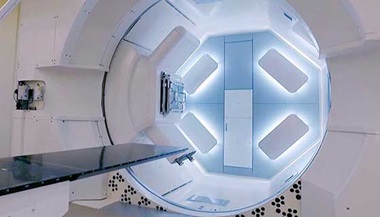
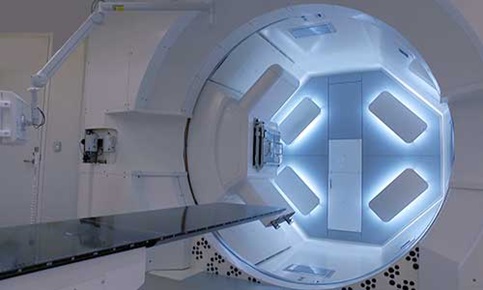
>> Narrator: At 16 feet in diameter, this particle accelerator, the synchrotron, uses a ring of small magnets to spin protons that come from hydrogen atoms up to two thirds the speed of light. The protons are injected into the ring, accelerated to energies between 70 and 230 MeV, and then extracted to the synchrotron and transported to each of the treatment rooms. The 80,000 square foot proton center contains the synchrotron, a space for research, and three treatment rooms used for adult and pediatric patients. Proton beams travel down a beam line nearly 50 yards long, and enter one of four rooms. An organized assembly of electromagnets focuses the proton beam toward the gantry. Nearly three stories high, a large mechanical arm called a gantry can move the beam 360 degrees around the patient, treating the tumor from several angles as it destroys tumor cells layer by layer. 3D imaging built into the gantry with cone beam CT capability allows pinpoint precision in locating the tumor. A five-millimeter-wide proton beam, guided by a 21,000-pound magnet, is directed to the resting patient.
What are the benefits of proton therapy?
The key benefit of proton therapy is the ability to more precisely target the tumor cells. Research shows that proton therapy results in a higher dose of radiation to the tumor but significantly less radiation to healthy cells near the tumor. With less healthy tissue affected by the radiation, side effects may be milder, and there is less risk of developing secondary cancers due to radiation.
Thanks to this precision targeting, proton therapy offers additional benefits:
- Protecting important neurological functions like speech or memory when a tumor is close to the areas that control these functions
- Minimizing radiation to vital organs such us the heart and lungs when treating cancers of the breast or spine
- Reducing the risks for children with cancer, who often suffer lasting side effects from toxic cancer treatments
- Helping to avoid more radiation to areas that previously had radiation, in case a tumor comes back close to or in its original location
What are the disadvantages of proton beam therapy?
Proton therapy is not the right choice for everyone. Some negatives of proton therapy include:
- Availability: There is a small number of proton therapy centers in the U.S., which means you may need to travel for treatment that may last several weeks.
- Longer planning time: Your radiation oncologist will need a few weeks to plan proton therapy. They may recommend traditional radiation if you need treatment sooner.
- Insurance coverage/cost: Proton therapy costs more than photon radiation therapy because the machines and equipment for proton therapy are very complex, and they are expensive to make and operate. Some insurance providers may not approve proton therapy if there is no definitive evidence that it is a better treatment option. It is important to check with your insurance provider about coverage. Many proton therapy centers, including the center at Johns Hopkins, have insurance authorization specialists who can assist you in obtaining treatment authorization.
Proton Therapy for Head and Neck Cancer | Angie’s Story
Preparing for Proton Therapy
Proton therapy involves careful planning to make sure the proton beam hits its target and delivers the right dose of radiation. Many different specialists are involved in the planning and delivery of proton therapy, including:
- Radiation oncologists
- Nurses
- Social workers
- Dosimetrists
- Physicists
- Radiation therapists
Planning can take a few weeks, and includes:
- Imaging: You will have imaging tests such as a CT scan or MRI to confirm the location and size of the tumor. Using these scans, the radiation oncologist locates the tumor and uses a computer to map its exact shape and size, as well as important surrounding organs and tissues.
- Simulation: The imaging information also helps position your body for treatment. The care team might mark on your body where to aim the proton beam. These marks are small and mostly temporary, although some can be permanent. Once the right position is determined, a member of the team will create immobilization devices to help you maintain this position during each treatment. If an area of your head or neck is being treated, the team will create a special mesh mask custom-fitted to your face to keep your head from moving. You can see and breathe through the mask.
- Dose planning: The radiation oncologist determines exactly how much radiation to deliver to the target area. Dosimetrists use special computer programs to figure out the best way to deliver that dose, how to position the beam and how deep into the body the beam should travel.
- Quality assurance: Physicists perform a quality assurance check to make sure the proton beam can be generated to the exact dose, depth and angles needed for treatment.
What happens during proton beam treatment?
Proton therapy is an outpatient procedure performed in a specialized center. Most patients are treated over a course of several sessions, and some treatments take longer than others. The proton treatment takes place in a special room equipped with a large mechanical arm called a gantry that moves the proton beam around you as you lie on a table.
During a proton therapy treatment session:
- Your care team will place you on the treatment table in the position determined during the simulation stage. They will use positioning devices to hold your head and body still, such as a body mold or a mask.
- The radiation oncologist will position the gantry so the proton beam is lined up with the marks on your skin indicating the location of the tumor. The gantry is not a confined space like an MRI machine, so you should not feel claustrophobic during treatment, although you will have to be very still.
- An X-ray or another imaging scan will be taken to confirm that you are in the right position and everything is aligned.
- Radiation therapists will leave the room to operate the proton beam machine. A video camera helps the therapist see and hear you, so you will not be alone.
- Once the machine is on, the particle accelerator in a separate room speeds up protons and sends them to the gantry in the treatment room. The gantry focuses protons into a thin beam and aims them at the tumor. The gantry might move around your body to treat the tumor from different angles.
- The proton beam may turn on and off several times during treatment as it moves around or needs to realign with the tumor if it shifts as you breathe. You will not feel the proton beam entering the body or treating the tumor, but you might hear clicking noises as the machine moves around you.
How long do proton therapy treatments take?
Depending on the size, location and number of tumors, you can expect to spend about 15–30 minutes in the treatment room. The proton radiation treatment itself takes only a few minutes, but it takes time to position you and calibrate the machine before generating a proton beam. It could take an hour or longer for the entire appointment from the moment you enter the center until you leave.
Most patients need several treatments with proton therapy. Treatments could be daily, twice a day or less frequent, and often take multiple weeks. Your radiation oncologist will discuss the optimal treatment schedule with you.
Proton Therapy at Johns Hopkins
- Precise, personalized care delivered by leading experts.
- Ability to target hard-to-reach tumors.
- Care offered in Washingon, D.C.
Recovery After Proton Therapy Treatments
After being treated with the proton beam, most people can go home and resume normal activities. Your doctor might order tests to see how the treatment is affecting the tumor, and adjust the treatment if necessary.
Adults typically do not need to be under anesthesia (put to sleep) during treatment, so they can drive to and from appointments. Children often need sedation to help them keep still, so they may need to stay longer after treatment for the sedation to wear off.
Proton Therapy Side Effects
Proton therapy side effects are similar to those of traditional radiation therapy. Side effects can develop gradually after treatment, and may include:
- Sore, reddened skin in the area where the proton beam entered the body. It can look and feel like a sunburn.
- Hair loss in the treatment area
- Tiredness or low energy
Additional side effects, depending on the area treated, can include headaches and problems with eating and digestion.
Proton Therapy Versus Photon and Other Radiation Therapies
Unlike traditional photon radiation therapy that uses radiation in the form of X-rays or gamma rays, proton therapy uses proton particle radiation. Both photon and proton radiation damage the tumor’s DNA, but researchers say damage to the tumor cells caused by protons is more direct and harder to repair.
More importantly, protons only travel a certain distance into the body before they stop, and they deliver the highest dose of radiation at the end of their pathway. This burst of energy can appear on a graph as what is called the Bragg peak. Radiation oncologists plan proton therapy treatments so the maximum dose hits the tumor cells. In this way, proton therapy reduces radiation exposure and potential damage to healthy tissue, especially in sensitive areas such as the brain, eyes, spinal cord, heart, reproductive organs, major blood vessels and nerves.
In regular radiation therapy, such as photon therapy or gamma knife treatments, the beam of high-energy gamma rays or X-rays goes into the body, through the tumor and out the other side. Photons release energy along the entire path they travel, which means they radiate healthy tissues beyond the tumor. It is estimated that 30% to 40% of the photon dose passes through the tumor. This “exit dose” of radiation can damage the DNA of healthy cells. Proton therapy generates virtually no exit dose.
While the treatment effects of photon and proton radiation may be similar, the precision of proton therapy often makes it a safer choice with fewer aftereffects for certain types of tumors.
Proton Therapy | Targeted Cancer Treatment
What is the difference between proton therapy and SBRT, SRS and IMRT?
Depending on the number of treatments and the precision and intensity of radiation, radiation therapy has different names, including stereotactic radiosurgery (SRS), stereotactic body radiation therapy (SBRT) and intensity-modulated radiation therapy (IMRT). Traditionally, these terms describe photon radiation. There are certain differences between these treatments and proton therapy:
- SRS and SBRT, such as gamma knife and CyberKnife therapy, use numerous photon radiation beams pointed at the tumor from many angles to combine their effect at the point of intersection. Proton therapy typically uses fewer beams that move to hit the tumor from different angles. Importantly, proton therapy concentrates radiation on the tumor and has a smaller exit dose than photon radiation.
- SRS is usually delivered in a single high-dose treatment, and is often used to treat brain tumors. Proton therapy usually takes multiple treatments, even for brain tumors.
- SBRT refers to treating tumors outside of the brain (throughout the body). The radiation is delivered in multiple high-dose treatments. The term SBRT can be used to describe photon or proton therapy.
- IMRT splits a single radiation beam into smaller beams of varying intensity, which makes it possible to target the radiation to the shape of the tumor and deliver it more precisely. IMPT (intensity modulated proton therapy) is the equivalent of IMRT using proton therapy. IMPT has virtually no exit dose, and exposes less normal tissue to radiation than photon IMRT.
Proton Therapy Versus Carbon Ion Therapy
Carbon ion radiotherapy (CIRT) is similar to proton therapy, except it uses carbon ions instead of protons. Carbon ions are heavier than protons, so they can deliver more radiation to the tumor and cause more damage to cancer cells. International research shows promising results in cancer survival rates with carbon ion therapy. However, there are presently no centers in the U.S. that offer CIRT.