Patient Stories
Meet some of our former patients sharing their Johns Hopkins experience. Patient stories include treatment for:
Cochlear Implants and Hearing Conditions
-
Carol's Story
Cochlear Implant

-
Sarah's Story
Cochlear Implant

-
Children of the Johns Hopkins Cochlear Implant Center
Cochlear Implants

-
The Huegel Family
Cochlear Implant

-
Liam's Story
Complex Middle Ear Surgery

-
Joyce's Story
Cochlear Implant

-
Mateo's Story
Cochlear Implant

Facial Plastic and Reconstructive Surgery
-
Vincent’s Story
Craniofacial Reconstructive Surgery
-
Anthony's Story
Facial Paralysis

-
Amber's Story
Reconstruction After Mohs Surgery

-
Richard's Story
Hair Transplant Surgery

-
Jen's Story
Basal Cell Carcinoma and Nose Reconstruction

-
Rex's Story
Severe Sinus Disease and Reconstruction

-
Kathy's Story
Gracilis Free Flap Surgery for Facial Reanimation

-
Diana’s Story
Restoring Facial Symmetry

-
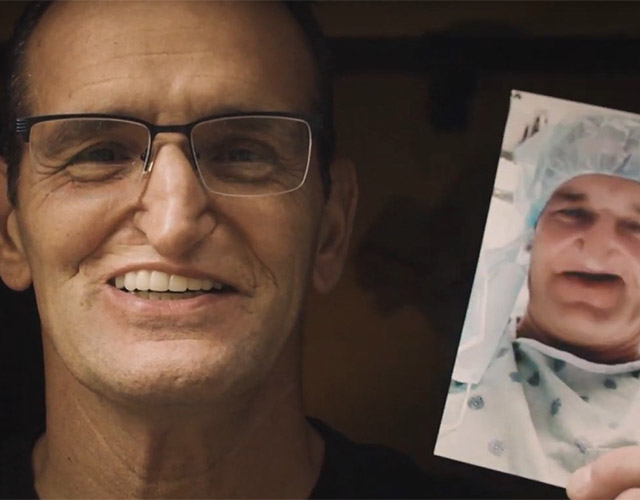
Scott's Story
Complex Microsurgical Facial Reconstructive Surgery

Oral, Head and Neck Tumors
-
Steve's Story
Oral, Head and Neck Cancer

-
Esther's Story
Salivary Gland Cancer
-
Jubenal's Story
Salivary Gland Tumor

-
Joe's Story
Oropharyngeal Cancer
-
Victor's Story
Oropharyngeal Cancer
-
David's Story
Oropharyngeal Cancer
-
Greg's Story
Oropharyngeal Cancer
-
Sam's Story
Oropharyngeal Cancer
Voice and Airway Conditions
-
John's Story
Tracheal Stenosis
-
Jessica's Story
Recurrent Respiratory Papillomatosis

-
Sandy's Story
Voice Cord Paralysis

Skull Base Tumors
-
Sofia's Story
Transnasal Endoscopic Surgery

-
Angie's Story
Olfactory Neuroblastoma

Sinus Conditions
-
Rex's Story
Severe Sinus Disease and Reconstruction

-
Dan's Story
Sinus Surgery and Sublingual Immunotherapy

-
Nici's Story
Sinus Surgery

Sleep Conditions
-
David's Story
Sleep Apnea

