Brain Tumors in Children
What You Need to Know
- Brain tumors are the most common solid tumors affecting children and adolescents, with close to 5,000 children diagnosed each year.
- Because of their location, some pediatric brain tumors and their required treatments can cause significant long-term impairment to intellectual and neurological function.
- Some forms of brain cancer can be life-threatening.
Transnasal Endoscopic Surgery | Sofia's Story
Diagnosed with a malignant skull base tumor declared inoperable by other surgeons, Sofia, a Connecticut teenager, came to Johns Hopkins and had her tumor removed with a transnasal endoscopic approach.
Symptoms of Brain Tumors in Children
The skull does not have excess room for anything other than the brain. Therefore, as brain tumors develop and expand, they cause extra pressure in this closed space. This is called intracranial pressure.
Increased intracranial pressure is caused by extra tissue in the brain as well as blockage of the cerebrospinal fluid flow pathways.
Symptoms include:
- Headaches
- Seizures
- Nausea and vomiting
- Irritability
- Lethargy and drowsiness
- Personality and mental activity changes
- Macroencephaly (enlarged head) in infants whose skull bones are not completely fused
- Coma and death, if left untreated
Brain tissue dysfunction caused by a growing tumor may cause other symptoms, depending on the tumor’s location.
For example, if a brain tumor is located in the cerebellum at the back of the head, a child may have trouble with movement, walking, balance and coordination. If the tumor affects the optic pathway, which is responsible for sight, the child may experience vision changes.
Brain Tumor Diagnosis in Children
A child experiencing brain tumor symptoms should be thoroughly evaluated by a pediatrician or pediatric neurologist, or in the emergency room to find the source of the problem.
The doctor’s evaluation usually includes imaging of the brain by an MRI scan. If the scan shows a brain tumor, the next step is a neurosurgical consultation. The pediatric neurosurgeon will work with the whole family to develop the best treatment plan for the child.
Other specialists may join the child’s treatment team, such as a pediatric oncologist (childhood cancer specialist), an ophthalmologist (if the child’s tumor affects the vision pathways), an epileptologist (to address seizures), a radiation oncologist, and advanced practitioners and technologists.
Tests for the Child with a Brain Tumor
In putting together the most appropriate treatment plan for a child with a brain tumor, the neurosurgery team will need to know:
- Tumor location: This is determined by a brain scan, using one or more types of imaging such as CT or MRI. Because there are many vital structures in the brain, there are places a tumor can grow that are not appropriate for surgery. The neurosurgeon’s careful evaluation will determine the accessibility of the tumor and the safest approach.
- Brain tumor type: Looking at the tumor cells under a microscope can reveal the brain tumor type, and give doctors insight on how the tumor is likely to grow or spread.
- Brain tumor grade: The grade refers to how aggressive the tumor cells appear to be. The higher the grade, the more aggressive the tumor.
Types of Brain Tumors in Children
Brain tumors can be categorized as:
Primary: Starting in the brain
Metastatic: Starting in other parts of the body and spreading to the brain
Benign: Slow-growing; non-cancerous. Benign tumors can still be difficult to treat if they are growing in or around certain structures of the brain.
Malignant: Cancerous. Unlike benign tumors that tend to stay contained, malignant tumors can be very aggressive. They grow rapidly and can spread to areas near the original tumor and to other areas in the brain.
Astrocytomas, Including Glioblastoma Multiforme
Astrocytomas are the most common type of glioma, accounting for about half of all childhood brain tumors. They are most common in children between the ages of 5 and 8.
The tumors develop from glial cells called astrocytes, most often in the cerebrum (the large upper part of the brain), but also in the cerebellum (the lower back part of the brain).
The grade of an astrocytoma is important. Your child’s treatment will be based on whether or not the tumor is slow-growing (low-grade, grade 1 or 2) or fast-growing (high-grade, grade 3 or 4). Most astrocytomas in children (80 percent) are low-grade. Sometimes they begin in the spine or spread there.
There are four main types of astrocytomas in children:
Pilocytic astrocytoma (Grade 1): This slow-growing tumor is the most common brain tumor found in children. Pilocytic astrocytoma is often cystic (fluid-filled). When this tumor develops in the cerebellum, surgical removal is often the only treatment necessary. Pilocytic astrocytomas growing in other locations may require other therapies.
Diffuse astrocytoma (Grade 2): This brain tumor infiltrates the surrounding normal brain tissue, making complete surgical removal more difficult. A fibrillary astrocytoma may cause seizures.
Anaplastic astrocytoma (Grade 3): This brain tumor is malignant. Symptoms depend on the location of the tumor. These tumors require a combination of treatments.
Glioblastoma multiforme (Grade 4): This is the most malignant type of astrocytoma. It grows rapidly, and often causes pressure in the brain. These tumors require a combination of treatments.
What Are the Most Common Childhood Brain Tumors? - On Call for All Kids
Other Pediatric Brain Tumors
Brain stem gliomas: Tumors in this location can be very challenging to treat. Most of these tumors are located in the middle of the brainstem and cannot be surgically removed, particularly the diffuse intrinsic pontine glioma, or DIPG. A few brainstem tumors are more favorably located and can be treated with surgery. These are often treated with non-surgical methods.
Choroid plexus tumors: These tumors are found in the choroid plexus — the part of the brain within the spaces in the brain, called ventricles, that makes cerebrospinal fluid, which surrounds and cushions the brain and the spinal cord. These tumors can cause a buildup of cerebrospinal fluid, resulting in hydrocephalus. They can be benign or malignant, and often require surgery as part of the treatment.
Craniopharyngiomas are benign tumors that occur near the pituitary gland.
Dysembryoplastic neuroepithelial tumors: These rare, benign tumors grow in the tissues covering the brain and spinal cord, and often cause seizures.
Ependymomas are another kind of glioma that forms from the cells that make, support, nourish, and line the ventricles (open areas of the brain’s interior that cerebrospinal fluid flows through). They require surgery plus radiation treatment in most cases.
Germ cell tumors: These tumors can be benign or malignant. They grow from germ cells, which form from eggs in women and sperm in men. During normal development of an embryo and fetus, germ cells usually become eggs or sperm.
Medulloblastomas: These malignant brain tumors account for about 15 percent of brain tumors in children. Medulloblastomas form in the cerebellum and occur primarily in children between the ages of 4 and 9, affecting boys more frequently than girls. Medulloblastomas can spread (metastasize) along the spinal cord. They typically require surgery plus other treatments.
Optic nerve gliomas: These tumors are found in or around the optic nerves — those that send messages from the eyes to the brain. Optic nerve gliomas are frequently seen in children with neurofibromatosis, a type of genetic disorder that affects the skin and nervous system. They can cause vision loss and hormone problems because of their frequent location near the base of the brain. These are typically difficult to treat due to the surrounding sensitive brain structures.
Treatment for Pediatric Brain Tumors
One or more of these approaches will be included in the child’s brain tumor treatment plan:
Surgery
Most brain tumors in infants and children require surgical removal, or at least a biopsy, as part of the treatment. The surgeon may recommend surgery to remove as much of the tumor as safely possible as a first step and to relieve intracranial pressure caused by the tumor. For low-grade or slow-growing tumors, surgery may be the only intervention necessary.
Follow-up Care after Surgery
The recovery process is different for each child. Children who received prompt diagnosis and treatment can do well after surgery.
Some pediatric patients may experience some temporary neurological deficits, such as muscle weakness. In most cases, this goes away shortly after surgery, unless there was substantial permanent damage before the child was diagnosed. Physical, occupational and speech therapy can help improve strength, function and speed of recovery.
Regular post-operative follow-up visits with the child’s neurosurgeon are also important to monitor neurological function and side effects from treatment, and to guard against recurrence of the tumor.
Radiation Therapy
This therapy focuses beams of high-energy radiation on the tumor tissue and a small amount of surrounding tissue. Some tumors, such as medulloblastoma, require additional radiation to the entire brain and spinal cord. Radiation is used very cautiously in infants and toddlers due to their growing brains.
Chemotherapy
Chemotherapy is used for many types of brain tumors including aggressive, high-grade tumors. Chemotherapy can be administered as pills (orally), intravenously (IV, by vein), injected directly into the cerebrospinal fluid, or injected directly into the cavity left after surgical removal of a brain tumor.
The Johns Hopkins Proton Therapy Center
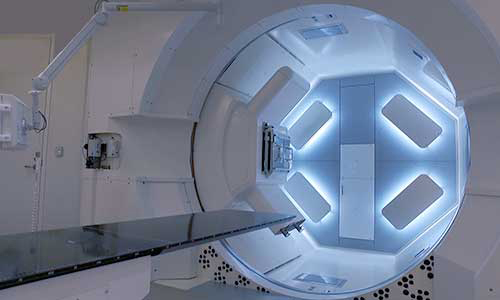
Proton therapy is used to treat certain tumors in children and adults. Our treatment center, located at Sibley Memorial Hospital in Washington, D.C., combines advanced proton therapy technology, the latest research and caring specialists.








