-
James Stuart Ferriss, MD

- Director, F.J. Montz Gynecologic Oncology Fellowship Program
- Associate Professor of Gynecology and Obstetrics
Expertise: Gynecology, Gynecologic Oncology
-
Kimberly Levinson, MD MPH

- Director of Gynecologic Oncology, Greater Baltimore Medical Center
- Associate Professor of Gynecology and Obstetrics
Expertise: Gynecology, Gynecologic Oncology
The Johns Hopkins F.J. Montz Fellowship in Gynecologic Oncology is a three-year program with one to two fellowship positions available each year. Our goal is to train world-class abdominal-pelvic surgeons, clinicians who are well-versed in medical oncology, palliative care and oncofertility for women with gynecologic malignancies, and the future academic leaders of our field.
Inside the Gynecologic Oncology Fellowship Program
James Stuart Ferriss, director of the F.J. Montz Fellowship in Gynecologic Oncology, describes our fellowship, a three-year program with one to two fellowship positions per year. As one of the strongest #GynecologicOncology programs in the country, we offer our fellows the opportunity to become well-versed in the spectrum of gynecologic oncology care by working in the lab, at the bedside and within the operating room.
Program Highlights
Surgical Breadth
Skilled and mature academic gynecologic cancer surgeons who have a proven commitment to excellence in patient care, academic pursuits, and education.
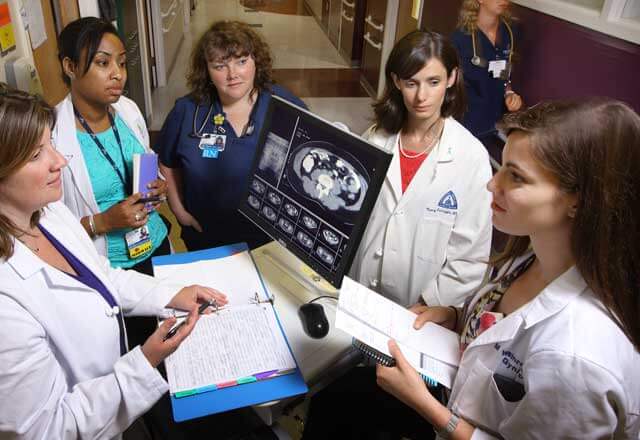
Multidisciplinary Collaboration
The full breadth and depth of expertise of the non-gynecologic oncologist faculty. These include medical oncologists, radiation oncologists, hepatobiliary surgeons, and gynecologic pathologists who are all experts within their respective fields.
Unique Research Opportunities
Faculty members who are full-time NCI scientist/investigators who bring not only a unique vision, but also access and exposure to resources to which fellows are rarely exposed.
Exposure to a Variety of Care Needs
Patient volume and mix, both of disease processes and socio-cultural demographics, such that the Fellow is fully exposed to all diseases that a Gynecologic Oncologist must be expert at managing.
Dedicated Academic Time
Dedicated and protected academic time for fellows each Friday from 0900-1200.
Discover More
Spend "discovery" block time in one of numerous disciplines: public health, cancer control and prevention access to care, outcomes research, international women's cancer care (focus on developing countries), health care financing, basic and translational laboratory sciences, growth factor and bio-marker expression and oncogenesis and cancer immunology and vaccine development.
Current Fellows
Alison Goulder, M.D.
Third Year Fellow

Benjamin Matthews, M.D.
Third Year Fellow

Tullia Rushton, M.D.
Second Year Fellow

Dana Lewis, D.O.
First Year Fellow

Emily MacArthur, M.D.
First Year Fellow

Requirements
Completion or anticipated completion of a ACGME accredited Gynecology and Obstetrics residency.
The FJ Montz Fellowship in Gynecologic Oncology is committed to cultivating and sustaining an environment that fosters the development of physician leaders who are committed to eliminating the nation’s health inequities through patient care, education, advocacy, and research. Diversity, equity, and inclusion are core values of our education program, the Department of Gynecology and Obstetrics, and the Johns Hopkins University School of Medicine. Applicants from backgrounds underrepresented in medicine are encouraged to apply! According to the AAMC, “Underrepresented in medicine means those racial and ethnic populations that are underrepresented in the medical profession relative to their numbers in the general population.
How to Apply
If you wish to apply to our fellowship program, please apply through ERAS at: http://www.aamc.org. Please include the following three letters of recommendation with your application:
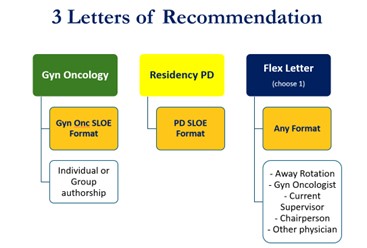
Please note the letters must be submitted via ERAS (to be included with your application). The Society of Gynecologic Oncology (SGO) offers a Standardized Gyn Onc SLOE and a Standardized Residency PD/Supervisor SLOE You will use the forms for two of your letters. Note: you only need to submit two standardized letters, the third letter can be either standardized or traditional format.
If you should have any questions, please feel free to contact us:
Phone: 410-955-8496
Deadlines for 2024
The application deadline will be Monday, April 1, 2024.
We will send invitations to select applicants for interviews on Friday, April 26, 2024. We will only offer one invitation for each interview slot we have; thus, we will maintain a waiting list of highly qualified applicants. In accordance with updated NRMP guidelines, candidates will have 48 hours to respond to an interview request before we make an offer to another qualified candidate.
All interviews will be conducted via live video link. There will be no in-person events planned in Baltimore. Additional information will be shared as we get closer to our interview day.
Curriculum Details
Our fellowship is in excellent standing, with continuing accreditation received by the Accreditation Council of Graduate Medical Education (ACGME).
-
One to two fellowship positions offered each year.
-
Three years with an emphasis on progressive responsibility:
The fellow will be given progressively more responsibility throughout the Fellowship within the limitations imposed by the fellow's own capacities. Fellows in the latter half of their second clinical year will be performing a greater part of the more complex surgeries and will, in many instances, be the principal surgeon. There is no formal progression in responsibility of the fellows as regards their pivotal role as Leader of the Inpatient Care Team: this responsibility is the same the first month as it will be the last month that the fellow is on service. However, the amount of micro-management that the Attending of the Day performs will become less as the fellow proves themselves skillful in inpatient care.
-
Opportunities to conduct bench research in basic science/translational sciences are possible in the research year. As an alternative, research fellows may consider obtaining a Masters in Public Health (MPH) at the prestigious Johns Hopkins Bloomberg School of Public Health or a Masters in Business Administration (MBA) at the Johns Hopkins Carey School of Business. Enrollment into a masters program is not guaranteed, and will require submission of a proposal that demonstrates how the degree will impact long term career plans.
Medical Oncology/Chemotherapy:
- Half-day clinic, each week (Mentors: Deb Armstrong and Stephanie Gaillard)
The research program is tailored depending on the interests and career goals of the fellow. Clinical research projects are facilitated throughout the fellowship experience by prospective and retrospective clinical databases, including institutional databases, larger national databases, as well as a robust tumor bank.
The fellow is expected to develop, complete, and present at least two research projects under the mentorship of an identified faculty member(s). With supervision, the fellow will be expected to develop both short-term and year-long research projects. Goals for these studies include at least:
- 2 posters or oral presentations at national meetings
- 2 manuscripts prepared for journal submission and accepted for publication in a peer review journal by graduation
The average number of manuscripts accepted for publication per fellow in our program is 6 (and select fellows have many more). Almost all fellows will have the opportunity to present their work orally at a regional or national meeting. Fellows will be funded for travel to attend at least 1 national meeting for presentation per year, and often have the opportunity to attend more conferences.
-
Gynecologic Pathology:
- 2 weeks (Mentors: Russell Vang and Deyin Xing)
Weinberg Intensive Care:
- 4 weeks (Mentor: Pamela Lipsett)
-
Palliative Care:
- 2 weeks (Mentors: Thomas Smith and Deborah Doberman)
Radiation Oncology:
- 2 weeks (Mentor: Akila Viswanathan)
Surgical Oncology (optional)
-
Please click here to view a PDF of our rotation block schedule.
-
Fellows have the option of designing a customized rotation in concert with the program director.
Teaching of Residents and Students:
Though teaching obligations are predominantly the responsibility of the attending faculty members, serving as a resident and student educator is also expected of the fellow. As the inpatient team leader, it is anticipated and expected that the fellow will serve as a teacher of inpatient management skills for the residents and medical students on the service, and impart basic gynecologic oncology knowledge. The fellow will also be invited to present resident lectures at the resident school time two or three times a year.
Benign Gynecology:
The fellow will not be participating in the care of patients with benign gynecologic diseases except those that are admitted by the Kelly Gynecologic Oncology Service attendings or the gynecologic oncology service at Greater Baltimore Medical Center. Further, the fellows will not take obstetrics service attending calls—either in the hospital or out—and will not staff benign gynecology clinics or consultation suites.
Lectures:
Along with resident school time lectures, the fellows will occasionally lecture at the Departmental Grand Rounds. The fellows will also be invited to give lectures for student clerkships, institutional continuing medical education conferences and for select national continuing medical education courses.
-
Unique resources available at the Johns Hopkins Hospital and Medical Institutions:
- Johns Hopkins University Bloomberg School of Public Health
- Johns Hopkins Program in International Education in Gyn/Ob (JHPIEGO)
- Johns Hopkins University Carey Business School
- Proximity to the NCI
- Sheikh Zayed Critical Care Tower at Johns Hopkins Hospital has 355 private rooms, state of the art imaging, surgical technology and operating rooms and a beautiful new labor suite. The Zayed Tower offers the opportunity for enhanced educational opportunities for gynecologic oncology fellows and a modern healing environment for patients.
- The operating rooms are equipped with state of the art laparoscopic equipment, surgical beds and eight da Vinci surgical robotic platforms.
- NCI designated Comprehensive Cancer Center with all of the anticipated shared core-facilities, which is part of the National Comprehensive Cancer Network.
- Total integration of the Training Program into the Johns Hopkins Hospital and Medical Institutions (JHMI)-Greater Baltimore Medical Center (GBMC) Gynecology and Obstetrics universe.
- Minimal distance (9.5 miles) and travel time (20 minutes during peak traffic volume) between facilities
- A relatively inexpensive community in which to live.
- The cultural and geographic advantages of the Greater Baltimore-Washington area.
- The high quality of JHMI residents.
The Program Director, Dr. James Stuart Ferriss and Associate Program Director, Dr. Kimberly L. Levinson are responsible for the continuous supervision of all fellows with support from Sarah Meyers, Fellowship Program Coordinator for Oncology and Maternal Fetal-Medicine. Throughout the three years of the fellowship, the fellows meet with the program director on a regular basis. Additionally, fellows will be supervised by some of the following individuals when they are either on a specific rotation or participating in protected discovery time.
Sarah Meyers
Fellowship Program Coordinator for Oncology and MFM
Email: [email protected]
Phone: 410-955-8496
Deborah K Armstrong, MD

- Director, Breast and Ovarian Surveillance Service
- Professor of Oncology
Expertise: Medical Oncology
Stephanie Gaillard, MD PhD
- Director of Gynecologic Cancer Trials
- Associate Professor of Oncology
Expertise: Medical Oncology
Russell S. Vang, MD

- Director, Division of Gynecologic Pathology In-house Service
- Professor of Pathology
Expertise: Clinical and Laboratory Pathology
Pam A. Lipsett, MD

- Program Director, Surgical Critical Care
- Professor of Surgery
Expertise: General Surgery
Geoffrey Neuner, M.D.
Akila Viswanathan, MD MPH
- Director, Johns Hopkins Radiation Oncology and Molecular Radiation Sciences
- Professor of Radiation Oncology and Molecular Radiation Sciences
Expertise: Radiation Oncology
Tom J. Smith, MD

- The Harry J. Duffey Family Professor of Palliative Medicine
- Professor of Oncology
Expertise: Hospice and Palliative Care, Medical Oncology