Stem Cell Signal Drives New Bone Building
01/07/2019
“Our bones have a limited pool of stem cells to draw from to create new bone,” says Aaron James, M.D., Ph.D., associate professor of pathology at the Johns Hopkins University School of Medicine, and the study’s senior author. “If we could coax these cells toward a bone cell fate and away from fat, it would be a great advancement in our ability to promote bone health and healing.”
The regenerative group of cells, known collectively as stem cells, all have the potential to develop into a variety of cell types including those that make up living tissues, such as bones. Scientists have long sought ways to manipulate the growth and developmental path of these cells, in either a living animal or the laboratory, to repair or replace tissue lost to disease or injury.
Previous studies by others, James points out, showed that a particular type of stem cell — perivascular stem cells — had the ability to become either bone or fat and numerous studies since then have focused on advancing the understanding of what signaling proteins drive this developmental change.
From past studies of his own, James also knew that the protein WISP-1 plays a key role in directing the stem cells.
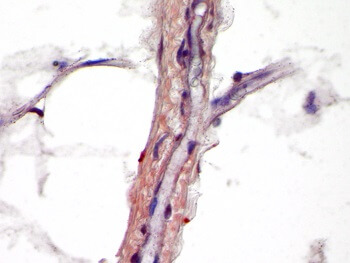 |
WISP-1 protein (purple) in human blood vessels. |
In his new experiments, James and his team genetically engineered stem cells collected from patients to block the production of the WISP-1 protein. Looking at gene activity in the cells without WISP-1, they found that four genes that cause fat formation were turned on 50–200 percent higher than control cells that contained normal levels of the WISP-1 protein.
The team then engineered human fat tissue stem cells to make more WISP-1 protein than normal, and found that three genes controlling bone formation became twice as active as in the control cells, and fat driving genes such as peroxisome proliferator-activated receptor gamma (PPARγ) decreased in activity in favor of “bone genes” by 42 percent.
With this information in hand, the researchers next designed an experiment to test whether the WISP-1 protein could be used to improve bone healing in rats that underwent a type of spinal fusion — an operation frequently performed on people to alleviate pain or restore stability by connecting two of the vertebrae with a metal rod so that they grow into a single bone. An estimated 391,000 spinal fusions are performed in the U.S. each year, according to the U.S. Agency for Healthcare Research and Quality.
“Such a procedure requires a massive amount of new bone cells,” says James. “If we could direct bone cell creation at the site of the fusion, we could help patients recover more quickly and reduce the risk of complications.”
In their experiments, the researchers mimicked the human surgical procedure in rats, but in addition, they injected — between the fused spinal bones — human stem cells with WISP-1 turned on.
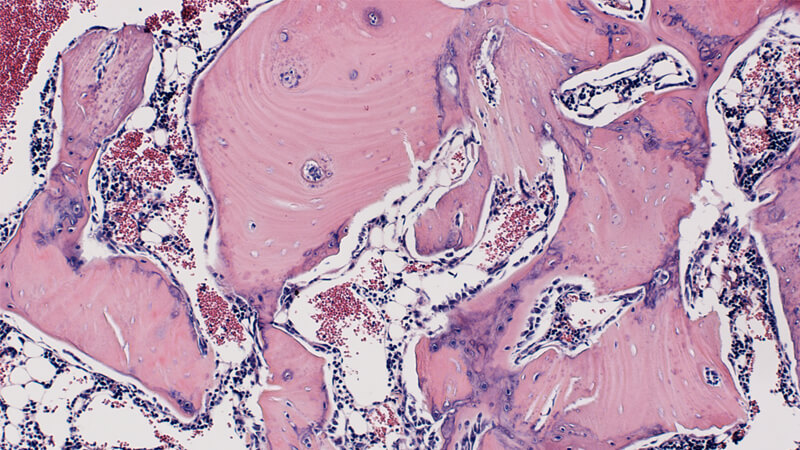
After four weeks, the researchers studied the rats’ spinal tissue and observed continued high levels of the WISP-1 protein. They also observed new bone forming, successfully fusing the vertebrae together, whereas the rats not treated with stem cells making WISP-1 did not show any successful bone fusion during the time the researchers were observing.
“We hope our findings will advance the development of cellular therapies to promote bone formation after surgeries like this one and for other skeletal injuries and diseases, such as broken bones and osteoporosis,” says James.
According to the Office of the Surgeon General, 1.5 million Americans suffer fractures from bone disease every year. James cautions that while transplanting stem cells to affected bones to help them heal is an increasingly popular therapeutic goal, it has not yet been proved safe or effective in humans.
The researchers also plan to explore whether reducing the level of WISP-1 protein in stem cells could preferentially favor the development of fat cells for soft tissue wound healing as well.
Other researchers involved in the study include Carolyn Meyers, Jiajia Xu and Kristen Broderick of the Johns Hopkins University School of Medicine. Additional authors on the paper include Greg Asatrian, Catherine Ding, Jia Shen and Kang Ting from the University of California, Los Angeles (UCLA), and Chia Soo and Bruno Peault from UCLA and Orthopaedic Hospital Research Center.
The study is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01 AR070773, R01 AR061399, R01 AR066782, K08 AR068316), the Department of Defense (W81XWH-18-1-0121, W81XWH-18-1-0336), the American Cancer Society (Research Scholar Grant, RSG-18-027-01-CSM), the Maryland Stem Cell Research Fund and the Musculoskeletal Transplant Foundation.
The authors declared competing interests: Ting, Soo and Peault are inventors of perivascular stem-cell-related devices with patents filed from UCLA. Ting and Soo are founders of Scarless Laboratories, which sublicenses perivascular stem-cell-related patents from the University of California Board of Regents, and they hold equity in the company. Soo is also an officer of Scarless Laboratories.
