
Arnold Simon
Little more than a year since his diagnosis with pancreatic cancer that had spread to his liver, 68-year-old Arnold Simon’s cancer is gone. This outcome is almost unheard of with any advanced cancer, let alone advanced pancreatic cancer, overall one of the deadliest types of cancer. Achieving these kinds of unprecedented results for patients is the mission of the new Precision Medicine Center of Excellence for Pancreatic Cancer, one of the first at Johns Hopkins.
It wasn’t a coincidence that Simon beat the odds. A clinical trial developed by pancreatic cancer expert Dung Le, M.D., testing a low-dose combination of five drugs—four that had already demonstrated an ability to attack pancreatic cancer cells and one that most considered ineffective for the cancer—was aimed at helping patients with advanced pancreatic cancer.
Le believed combining drugs that had shown some ability to kill pancreatic cancer cells would multiply the effect against the cancer. To make the drug combination an option for patients required some creativity. Each drug has its own toxicities, so combining the drugs at standard doses would multiply toxicities and be too harmful to patients, explains clinical research nurse manager Katrina Purtell, R.N., who collaborates with Le on the multidrug trial funded by Swim Across America. Le decided to try the drugs at lower doses.
Le based her hunch on laboratory evidence that the power of the five drugs at lower doses would be greater than the higher doses of any one of the drugs alone. Simon has no doubt that he is a pancreatic cancer survivor because of Le’s ingenuity. “No one else thought of putting these drugs together like this,” he says.
What makes a treatment work in one patient and not another is central to precision medicine and directing patients to therapies that will help them and away from ones that won't.
— Dung Le, M.D.
This new trial, and many others aimed at improving pancreatic cancer survival, are derived from years of science, and the new Precision Medicine Center of Excellence is tasked with advancing this progress more quickly. The Precision Medicine Center is directed by Christopher Wolfgang, M.D., Ph.D., one of the world’s leading pancreatic cancer surgeons, and clinician-scientist Lei Zheng, M.D., Ph.D., who is developing novel strategies to prompt the immune system to attack pancreatic cancer.
“Our research has shown that most cancers will require multiple agents to alter or interfere with the multiple signals that drive cancers,” says Zheng. “But what if we had an assay to predict the patients’ response to one specific component or a combination of components among the five drugs we would be able to further lower the toxicity and treat the cancer more precisely. This is what precision medicine is all about. Getting patients just the right treatment—not too much and not too little.”
Much of clinical cancer research has been based on giving patients the “highest tolerable dose” of anti-cancer drugs to kill as many cancer cells as possible. This approach has dominated clinical cancer research and drug discovery for decades, but Zheng and Wolfgang believe precision medicine is surely shifting this paradigm.
Precision medicine-based, targeted therapies are more about reprogramming cancer cells to behave like normal cells by zeroing in on a specific defect or defects in cancer cells or cells supporting cancer’s growth and interfering with the cells’ ability to communicate cancer-promoting signals. This shifts away from the high-dose therapies that essentially blanket the body with poisons, killing cancer cells but also many normal cells. More recent research has shown that less can be more when it comes to these targeted cancer therapies. Le, Zheng, Wolfgang and colleagues are finding that some drugs work as well, or better, at lower doses, and these lower doses usually translate to less collateral damage to normal cells, which means fewer side effects for patients. In a disease such as cancer that has been defined as much by its life-threatening nature as the quality of life-altering side effects of its treatment (infection risk, nausea, hair loss, fatigue), this is huge progress.
Of the 50 patients Le has treated so far with the experimental drug combination, three others had responses similar to Simon and were able to have their pancreatic tumors surgically removed.
“This is not the type of outcomes we have seen in the past, but it’s exactly the direction we expect precision medicine approaches to take us,” says Wolfgang. Exciting new therapies that make inoperable pancreatic cancers operable offer opportunities to transform the trajectory of advanced pancreatic cancers.
Zheng and Wolfgang also want to understand what is different about the four cancers that converted from in- operable to operable and the varied response in the 46 other patients. “What makes a treatment work in one patient and not another is central to precision medicine and directing patients to therapies that will help them and away from ones that won’t,” says Zheng. “There is no one size fits all when it comes to cancer treatment.”
Le and collaborators will use precision medicine research models to go back to the laboratory to learn why patients like Simon had such dramatic responses while others did not. They will look for biomarkers, identifying characteristics within pancreatic cancer cells and other cells near and around tumors that can help differentiate responders from nonresponders.
“If we know a subset of pancreatic cancers act in a certain unique way, we can look for a biomarker that rep- resents this subset,” says pathologist Robert Anders, M.D., Ph.D. “Then, when new patients come in with the same marker, we’ll understand how that cancer is going to act and what treatment to give. We may even be able to figure out how to convert a different cancer to behave more like one that responds to treatment.”
In Simon’s case, Wolfgang believes it may be a mutation in a gene known as BRCA that gave the multidrug therapy an edge against his cancer. Le added the drug cisplatin to her combination, a drug that is not typically used to treat pancreatic cancer. Recent research by Wolfgang found that platinum-based chemotherapy, like cisplatin, is linked to better survival rates in patients with BRCA1 or 2 mutations.
This latest finding builds upon an earlier discovery by Scott Kern, M.D., an expert in genetic alterations in pancreatic cancer, and Ralph Hruban, M.D., director of the Sol Goldman Pancreatic Cancer Research Center, that linked BRCA mutations to pancreatic cancer. Kern also showed that cancer cells containing BRCA mutations might be sensitive to cisplatin. Mutations to these genes are often inherited and more common among people of Ashkenazi Jewish decent. The genetic alteration increases the risk of developing certain types of cancer, including pancreatic cancer. Simon is Jewish, and closer examination of his cancer showed it contained a BRCA mutation.
Precision medicine bridges the laboratory and clinic, often with targets for treatment identified from laboratory exploration of the inner workings of the pancreatic cancer cell being matched to available drugs that hit these targets. There is much back and forth as clinicians and scientists work together to identify cancer’s vulnerabilities and develop therapies that exploit them.
“The interconnectivity of the lab- oratory and clinic to allow the quick translation of research findings to clinical care is a key characteristic of precision medicine,” says Wolfgang.
The Path to Precision
Decades of research and advanced technologies have gotten us to this point. They provide a new vantage point that affords scientists the ability to isolate and explore all components of cancer cells and the supporting cast of cells—the genetic hardware and the chemical software—to uncover the culprits that drive pancreatic cancers and expose vulnerabilities that can inform new treatments. These drivers include gene mutations or physical changes to the instruction manual that tell cells how to behave, epigenetic alterations or chemical changes to the DNA that also alter cell behavior, cancer’s ability to evade the immune system and the immune system’s willingness to tolerate cancer, and an entire microsociety around tumors that can cause cancer- inciting inflammation or help provide nutrients and other products essential to cancer cell survival. Each of these guides the treatment plan and is the basis of precision medicine approaches.
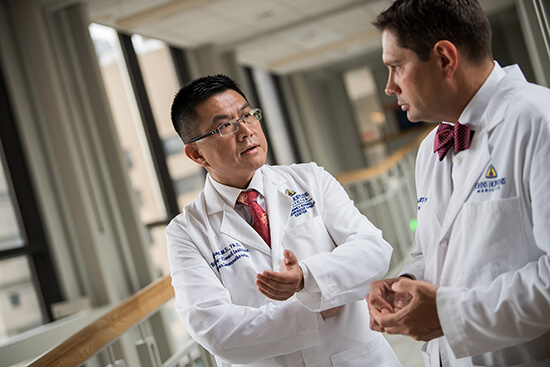
Lei Zheng, M.D., Ph.D., and Christopher Wolfgang, M.D., Ph.D.
“We are tailoring what we do based on the biology of the tumor, but there is much more to this than technology and information. It’s also our multispecialty collaboration that allows us to move beyond simply accumulating information to using it wisely to make a difference for patients,” says Zheng. “We have the expertise to understand what things are actually driving the cancer so that we can match available drugs to actionable targets. This is essential because attacking a target that is not influencing a cancer is not of much use and can actually be damaging.”
Sophisticated computer databases help marry the laboratory data to the human data, taking into account treatment outcomes, side effects, length of response, recurrences and other survival trends to arrive at the most effective and least toxic therapies.
“Our experts are uniquely positioned to make progress because much of the science that inspired precision medicine unfolded here,” says Zheng.
In 2008, Kimmel Cancer Center experts completed the genetic blue- print for pancreatic cancer, mapping out all the mutations in known human genes linked to cancer that make proteins that tell cells how to behave. The discovery uncovered an unexpected terrain of diversity in alterations from tumor to tumor. It explained why seemingly similar cancers often responded very differently to the same treatments. Still among the diversity were also some commonalities. Most of the mutations occurred in the same gene pathways, connected interactions that may conspire to promote cancer.
“This was the launching point for precision medicine,” says Wolfgang. “We could now use genetics to guide treatment and measure its effective- ness. We could drill down to the molecular level to look for alterations to target with drugs and determine if microscopic cancer cells, invisible in imaging, remained after surgery that could seed a recurrence without additional treatment.”
With the genetic blueprint of pancreatic cancer complete, other re- searchers could begin to probe deeper and create a more complete picture of pancreatic cancer from origin to metastasis. This work expands oppor-tunities to earlier detection and possibly, one day, prevention.
Clues Inside the Cell

Alison Klein, Ph.D., a researcher in the Sol Goldman Pancreatic Cancer Research Center, studies common gene variations that sometimes lead to pancreatic cancer.
“Most people who have them will never develop pancreatic cancer, but studying these changes can help us understand why some people develop the cancer,” says Klein. “Combining this information with other data we have on pancreatic cancer may help us figure out who is most at risk.”
Although Le’s multidrug treatment shows the promise to convert inoperable pancreatic cancers to operable, Wolfgang hopes precision medicine may also lead to earlier detection, before the cancer has spread. He and Klein are part of a team that developed a blood test that spots tumor-specific DNA and protein biomarkers of early-stage pancreatic cancer. Tumors tend to shed their mutated DNA into the bloodstream, making it possible for scientists to use gene-sequencing technology to sift through the blood and fish out DNA molecules specific for cancer amid a wide sea of normal DNA circulating in the blood.
Wolfgang also helped develop a gene-based test that distinguishes harmless pancreatic cysts from cysts that are likely to become cancer. These fluid-filled cysts are found in more than 1 million patients each year who have undergone CT or MRI scans because of abdominal pain and swelling. Imaging and even examining the fluid inside the cysts does not provide precise markers for precancerous potential, he says.
“The combination of genetic tests and clinical evaluation of patients’ cysts may change the way we guide patients on whether surgery to remove cysts is necessary,” says Wolfgang. “A panel of genetic markers, combined with clinical expertise, can accurately differentiate among types of pancreatic cysts and identify cysts that are safe to watch over time and cysts that need to be removed.”
Wolfgang, who leads one of the busiest pancreatic surgery programs in the world, credits his patients with helping pioneer these types of pancreatic cancer precision medicine approaches. “They have willingly provided the tumor samples scientists studied to identify the molecular changes that cause pancreatic cancers to form and grow,” he says.

Elizabeth Jaffee, Daniel Laheru and Beth Onners hosted long-term pancreatic cancer survivors, providing tours of the laboratory where the treatments that saved their lives were invented.
The Skip Viragh Center
This convergence of science, technology and clinical care that is accelerating progress against pancreatic cancer patients is rooted in the Skip Viragh Center for Pancreas Cancer Clinical Research and Patient Care. It is the model for multispecialty care, as one of the first to bring all the experts together to offer newly diagnosed patients a comprehensive consultation involving all the specialists contributing to the treatment and diagnosis of pancreatic cancer. Patients and experts partner to come up with the best treatment approach.

Daniel Laheru, M.D., and patient Nancy Azzaro
“I don’t think there is another place in the world set up to provide this kind of care,” says Daniel Laheru, M.D., co-director of the Skip Viragh Center. “Every patient who comes to us receives individualized care. For some, treatments are based on molecular markers from the onset. Other patients may receive standard of care, and if the treatment stops working or the cancer comes back, we can using molecular testing, imaging and all available tools to devise a new approach.”
More than 40 physicians, surgeons, research nurses and other staff members dedicated to pancreatic cancer make up the Skip Viragh Center. “We are making unheard-of progress in diagnosis, staging, research and individualized care,” says Elizabeth Jaffee, M.D., co-director of the Skip Viragh Center. “Everything that can be done for pancreatic cancer is being done in our Skip Viragh Center and Precision Medicine Center of Excellence for Pancreatic Cancer, and we are sharing with others so that our concepts can be used to help pancreatic cancer patients everywhere.”
Precision in Practice
Gene Ogle is among these patients. When he was diagnosed with pancreatic cancer at age 54, his first question was, “How long do I have to live?” His father died 30 years earlier of the same disease.
“My father died two months after he was diagnosed. My knowledge was that it was incurable and killed quickly,” says Ogle.
The multidisciplinary team of experts recommended surgery, specifically the Whipple procedure, a complex pancreatic cancer surgery refined by John Cameron, M.D., Wolfgang and other Johns Hopkins surgeons. They also told him about a clinical trial studying a pancreatic cancer vaccine developed by Jaffee that could be administered in the weeks leading up to surgery. The goal of the vaccine is to attract cancer-killing immune cells to the tumor to prevent the cancer from coming back after surgery. The trial, led by Zheng, was aimed at de- creasing the high rate of cancer recurrence caused when microscopic cancer cells break away from the tumor and travel through the bloodstream to other parts of the body. The vaccine would teach the immune cells to recognize pancreatic cancer cells and go after them wherever they are located in the body.
“Enrolling in the vaccine trial was an easy decision for me, and I have never regretted it one time,” says Ogle, who adds that he still didn’t have much hope for long-term survival.
Seven years, a 60th birthday celebration and two grandchildren later, he says: “My perspective is changing. I am so thankful that I lived to see these things. I didn’t think I would, but I’m beating this disease, and that’s a message people need to hear.”
He’s not the only one. The Skip Viragh Center recently hosted a luncheon for other long-term survivors and their families. In many ways, these patients are the founders of precision medicine. Their experiences are guideposts, as researchers and clinicians work together to reveal the cellular reasons for their remarkable responses. They provide real-life testimony to why Johns Hopkins leadership selected pancreatic cancer as a Precision Medicine Center of Excellence.
These types of unprecedented success stories are the result of collaborative laboratory and clinical research, and demonstrate what is possible when innovative science, medicine and technology are connected.
Kathleen Dowell, Donna Bender, Morris Campi and Manuel Rodriguez are members of an exclusive club—pancreatic cancer patients who have defied the odds. Blood and tumor samples they provided during their treatment are helping our experts understand why and how, and have led to precision medicine approaches being studied today. For Zheng and Wolfgang, these patients are living proof that curing pancreatic cancer is possible.
“The goal of the Precision Medicine Center of Excellence for Pancreatic Cancer is to make these kinds of out- comes the norm,” says Zheng.
The group toured Jaffee’s lab and saw firsthand how their blood and tissue samples are used in research, and how this research is improving treatments for pancreatic cancer patients today.
Dowell, who was diagnosed in 1997, recalled recovering from her Whipple surgery and thinking about the grim survival statistics for pancreatic cancer patients when she learned about the vaccine. She received just two injections, the fewest of anyone on the study, but had the most significant immune response.
Rodriguez, like Dowell, received Jaffee’s vaccine and is also a 20-plus year survivor. He came to the Kimmel Cancer Center after a surgeon at the community hospital near his Florida home told him that he had no chance of survival. Blood samples he provided revealed a unique enzyme that may offer clues to his response and could also benefit other pancreatic cancer patients.
Bender, too, sought out the Kimmel Cancer Center, when doctors told her that, at best, she had a few years. Now, 16 years later, she was thrilled to spend time with the inventor of the vaccine where all the research was done.
“I always wanted to meet Dr. Jaffee,” says Bender. “She is my Wizard of Oz, doing something magical behind a curtain.”
Campi was told he probably had between a 2 and 5 percent chance of surviving. Now, 14 years later, the 85-year-old, who was treated with surgery, radiation therapy, chemotherapy and 10 years of vaccine therapy, has no signs of pancreatic cancer. He goes to the gym regularly and says he feels “pretty good.”
Dowell’s two injections versus Campi’s 10 years of therapy are pro- viding precious information that is helping researchers determine what types and combinations of therapies work and in whom, when to give them, and how long to give them.
“This is what precision medicine is about—putting all of these puzzle pieces together to create better therapies for patients,” says Zheng, who collaborates with Jaffee on new, better-working versions of the vaccine that exploit molecular clues uncovered through patient-provided blood and tissue samples. “We have leaders in surgery, immunotherapy, pathology, genetics and epigenetics research. New discoveries are being made as a result.”
The Immune Component
Jaffee, a leader in cancer immunology, is excited about promising new approaches that, like her vaccine, make the immune system recognize and attack pancreatic cancer.
“Immunotherapy is a form of precision medicine because each time we give a treatment, it’s not acting in the same way in each patient. It’s acting on that particular patient’s immune system,” says Jaffee. “How the immune system sees the cancer is unique in each patient.”
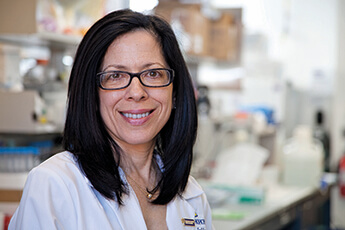
Jaffee, who is an associate director of the Bloomberg~Kimmel Institute for Cancer Immunotherapy, says Kimmel Cancer Center experts are leading the way, unraveling the science that led to her immune boosting pancreatic cancer vaccine and new immunotherapy drugs. With precision medicine in mind, they are developing biomarker tests that identify patients likely to benefit from immunotherapy and developing new ways to convert immune-resistant cancers to immune-responsive cancers.
Two new drugs called pembrolizumab (Keytruda) and nivolumab (Opdivo) are among a class of immunotherapies known as checkpoint inhibitors that release a brake cancer cells put on the immune response, allowing the immune system to do its job and attack cancer cells. The drugs work particularly well in cancers that contain a spell-checklike failure in their DNA called mismatch repair deficiency. This failure allows DNA errors to go uncorrected, initiating an accumulation of gene mutations and contributing to the development of many different types of cancer, including pancreatic cancer. The large numbers of mutations caused by mismatch repair deficiency make cancer cells look different from normal cells. Immune cells recognize this difference, much like they recognize foreign invaders, such as bacteria and viruses.
Le led a clinical trial testing pembrolizumab in patients with mismatch repair deficiency. The work led to FDA approval of the drug for any patient whose cancer contains this genetic repair defect, regardless of type or stage. It is the first time a cancer drug has been approved based on a specific genetic profile instead of a cancer type. This type of shift is at the core of precision medicine, where studies of new drugs are no longer in all patients with late-stage or aggressive cancers that do not respond to standard treatments. Instead, using biomarker tests, our doctors can identify patients whose cancers have the unique characteristics that portend a likely response to a drug and get the optimal therapy to patients upfront.
“It’s incredibly exciting that we now can prescribe pembrolizumab for patients with mismatch repair-deficient cancers. This could reach 2 to 3 percent of all advanced solid tumor patients. Given the potential for durable clinical benefit, we now have a reason to test for DNA mismatch repair deficiency in almost any cancer,” says Le.
The mismatch repair deficiency finding led Jaffee and two other Skip Viragh Center researchers, Mark Yarchoan, M.D., and Alexander Hopkins, Ph.D., to take another look at gene mutations and explore exactly how big an effect the number of mutations has on response to immune checkpoint inhibitors across many different cancer types. They analyzed more than 27 cancer types and found that mutational burden, or the number of gene mutations a cancer has, is the single most significant predictor of response to immunotherapy with checkpoint inhibitors.
“More than half of the differences in how well cancers responded to immune checkpoint inhibitors could be explained by the mutational bur- den of that cancer,” says Yarchoan.
Tumor mutations, typically viewed as the defining characteristic of the cancer cell because they cause a normal cell to turn malignant— giving it the ability to survive, grow and spread—are actually beneficial when it comes to immunotherapy.
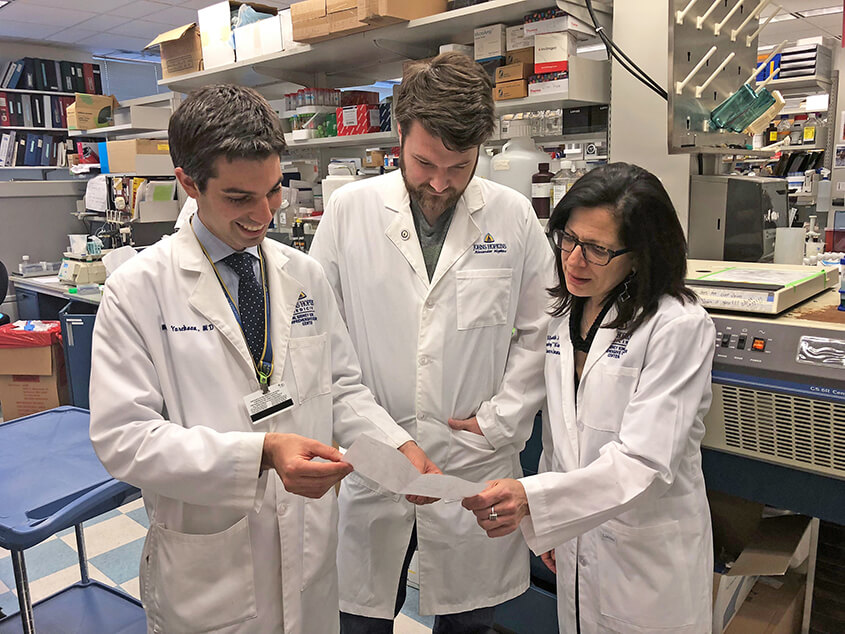
Mark Yarchoan, M.D., Alexander Hopkins, Ph.D., and Elizabeth Jaffee, M.D., developed a computerized tool that calculates the number of mutations in a tumor, a biomarker that can predict response to immunotherapy.
“The idea that a tumor type with more mutations might be easier to treat than one with fewer sounds a little counterintuitive. It’s one of those things that doesn’t sound right when you hear it,” says Hopkins. “But with immunotherapy, the more mutations you have, the more chances the immune system has to recognize the tumor.”
Jaffee, Yarchoan and Hopkins developed a computerized tool that calculates mutational burden to predict individual tumors most likely to respond to immunotherapy. Future studies might also focus on finding ways to prompt cancers with low mutational burdens to behave like those with higher mutational burdens so that they will respond better to these therapies.
“This is precision medicine— moving beyond what’s true for big groups of patients to see whether we can use information to help any given patient,” says Yarchoan.
Yarchoan, Le, Zheng and others are collaborating with Jaffee to use checkpoint inhibitors to augment the immune-boosting effect of her pancreatic cancer vaccine. The vaccine improves the immune response, recruiting many cancer-attacking T cells to the tumor site only to be signaled by cancer cells to stop.
Combining the vaccine with check- point inhibitors, and potentially other immune cell-stimulating drugs, may remove brakes on the immune response to the cancer.
Wolfgang is excited about mounting evidence coming from these clinical trials that shows giving a checkpoint inhibitor or vaccine and checkpoint inhibitor before surgery decreases the size of tumors and keeps cancers from returning.
Some cancers naturally attract the attention of cancer-killing T cells, but pancreatic cancer typically is not one of them.
“The vaccine is the first step in turning pancreatic cancer into an immune-responsive cancer. Once it gets T cells into the cancer, we can help them do their work by removing as many restraints as possible,” says Yarchoan.
Jaffee and Yarchoan believe the immune checkpoints cancer cells exploit to stop T cells from doing their job may vary among patients. “Potentially, we could customize what drugs we combine with the vaccine at an individual level,” says Yarchoan.
Jaffee has leveraged their pioneering pancreatic cancer research nationally. Since 2014, she has led a Stand Up To Cancer-Lustgarten Foundation pancreatic cancer Dream Team focused on developing new immunotherapies. Of the 22 Dream Teams, this is the only one that is female-led, and with Jaffee at the helm, top pancreatic cancers experts from 11 cancer centers are engaged in the collaboration, resulting in five new clinical trials and more than 600 patients treated.
Moving Forward
Simon, the patient who received Le’s multidrug regimen, still marvels at how quickly his doctors moved to help him. “They have a sense of urgency. I didn’t get that sense at other hospitals, ” says Simon. “I saw a surgeon on a Friday, had an appointment with Dr. Le the next Monday and began the trial two weeks later.”
Simon’s experience gets to the very heart of precision medicine. “I felt my health was more important to Dr. Le than her clinical trial and its results,” he says. “What was best for me was most important to her.”
Now, two years since receiving a dismal diagnosis of metastatic pancreatic cancer, Simon, a self-described “grumpy old Jewish guy,” is seeing things in a more positive light. Based on Le’s recommendation, he is now participating in another clinical trial for patients with inactive metastatic pancreatic cancer like his. The new treatment, as Simon describes it, “gets those lurking, hiding little cancer cells and zaps them before they get started.” The 68-year-old, who enjoys flying kites and bird-watching, is experiencing firsthand the power of precision medicine, and there is nothing more personal than that.
He wears a hat emblazoned with a large button that says, “Attitude is everything.” The button was a gift from a friend and fellow cancer survivor. He says it reflects his new positive outlook.
Jaffee gets it. “Pancreatic cancer patients are looking for hope,” she says. “Precision medicine is that hope.”
Contact our Precision Medicine Center of Excellence for Pancreatic Cancer at 410-933-PANC (7262).

