Socioeconomic disparities such as lower income and education levels are known contributors to adverse health outcomes and higher hospital admission rates among people with diabetes. They also may be risk factors for amputations associated with diabetic foot ulcers, according to a recent Johns Hopkins study. However, preventive, multidisciplinary care may offset the risk, researchers note.
Investigators, including several from the Multidisciplinary Diabetic Foot and Wound Service, reviewed Maryland Health Services Cost Review Commission database records of 7,415 patients with diabetes undergoing minor amputations (below the ankle) between 2012 and 2019. The odds of needing another amputation within a year were 23.6% overall, and were highest among those who were the most socioeconomically deprived. Results were published in the Journal of Surgical Research.
Vascular surgeon Caitlin Hicks, senior study author, says it’s likely due to a lack of good preventive care in this population.
“We know that adults with diabetes who have had foot ulcers in the past have a really high rate of recurrence, and the only way to avoid that is to have regular foot exams, good glucose control, and learn new gait patterns to avoid pressure in the area of the previous ulcer,” she explains.
A targeted, multidisciplinary approach addressing the health care needs of these patients may optimize care for this population, Hicks says. A previous study that the group published in the same journal showed wound healing to be largely dependent on wound characteristics and patients’ vascular status rather than patient demographics or socioeconomic factors. The study followed 277 patients with 621 diabetic foot wounds treated by the Johns Hopkins experts between 2012 and 2017. The group saw healing in 73% of wounds overall, regardless of patients’ socioeconomic status.
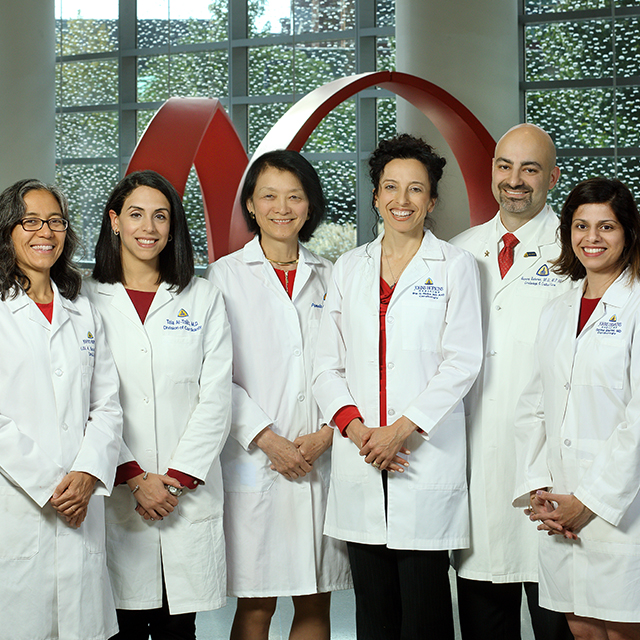
The Johns Hopkins service, started in 2012 under the direction of vascular surgeon Christopher Abularrage, features vascular surgeons, a surgical podiatrist, an endocrinologist, an infectious diseases specialist, a certified wound nurse and a physician assistant working together to manage both inpatients and outpatients presenting with foot wounds. Limb salvage is a key goal, with experts available to help control blood glucose, open blockages in arteries, prescribe antibiotics to decrease infections, and debride diseased tissue. A prosthetist works with patients to provide shoe inserts or leg braces as needed, and orthopaedic and reconstructive surgeons also are available.
“Once we get patients into our clinic and treat them for their first diabetic foot ulcer, we follow them regularly, so if they start to develop another wound we can address it immediately,” Hicks says.
Patients are informed upfront about the pathology and disease process of each wound and its potential to heal, adds podiatrist Ronald Sherman. They receive education and wound care supplies to take home until a home health nurse can visit. Experts with the service use the latest technologies in evaluating patients’ gait and in reconstructing the foot, he says.
“We treat every patient the same — as if they’re a member of our family,” Sherman says. “We have such a good service now, that if you come in with an advanced complex wound, you have probably a 95% chance of saving your leg. Around the country, it’s about 20% to 40%.”