Ada Graham, M.D., is a fellowship-trained colorectal surgeon with Johns Hopkins Medicine in the National Capital Region. The team, led by Vincent Obias, M.D., chief of colorectal surgery in the National Capital Region, focuses on complex colorectal needs.
Graham says her mission is to tailor each treatment plan to meet the individual goals of her patients, so they can get back to enjoying food, travel and life.
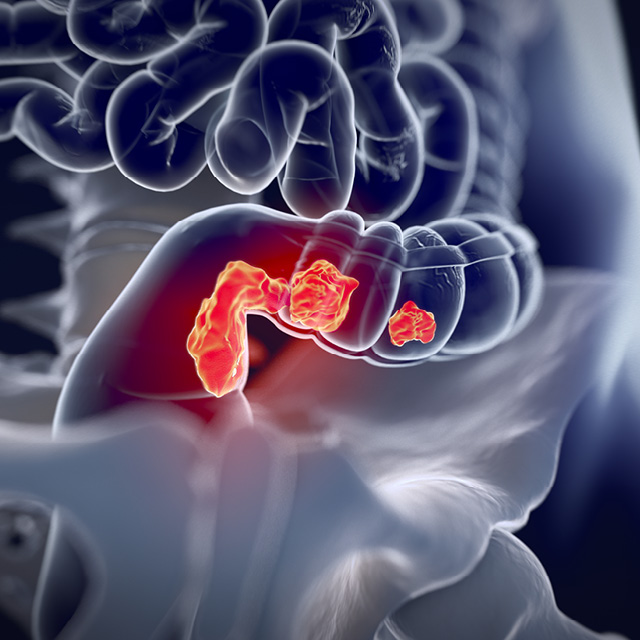
Graham, assistant professor of surgery in the colorectal surgery division, performs surgeries at Sibley Memorial Hospital and Suburban Hospital, treating cancerous and benign diseases including anal cancer, colon cancer, rectal cancer, inflammatory bowel disease and diverticulitis.
She also provides surgical relief for painful conditions including pilonidal disease, anal fistulas, hemorrhoids and anal fissures. Graham works closely with gastroenterologists to create a treatment course that is customized for each patient.
Her research focuses on inflammatory bowel disease (IBD), a chronic autoimmune condition that causes inflammation of the intestines and can take the form of either ulcerative colitis, which is confined to the large intestine, or Crohn’s disease, which can affect the entire digestive tract, from the mouth to the anus.
People with IBD tend to experience flare-ups that can include symptoms such as abdominal pain, diarrhea, rectal bleeding and fever. Over time, the intestines can become damaged, leading to abscesses, fistulas and increased risk of colon cancer. Most people with IBD are diagnosed before they turn 30, although some people develop IBD when they are in their 60s or older. IBD can run in families, and is more prevalent in people of Jewish ancestry.
Gastroenterologists can prescribe a broad variety of medications to manage inflammatory bowel disease, but some patients have disease progression despite aggressive medical therapy.
More than half of people diagnosed with IBD will benefit from surgery to remove damaged portions of the intestine, explains Graham. For these patients, surgery can significantly improve their quality of life. For patients with Crohn’s disease, she seeks to save as much bowel as possible. “I can cut out the damaged part and sort of reset the clock,” she says.
Most of the surgeries Graham performs are minimally invasive, she says, and compared with open surgery, require smaller incisions, which promote faster recovery and fewer complications. Patients are typically up and walking within a day of surgery, says Graham, a proponent of Enhanced Recovery After Surgery (ERAS), a protocol used at Johns Hopkins hospitals to help patients recover from surgery as quickly and comfortably as possible.
Graham, who graduated from Dartmouth College with a degree in linguistics and earned her medical degree at the University of Tennessee Health Science Center, describes herself as a careful troubleshooter and problem-solver.
Her background includes time as a park ranger in New Zealand, an English teacher in Thailand and a researcher studying language acquisition after stroke at the University of Chicago and the University of California-Irvine. She has also hiked mountains all over the world, including above the Arctic Circle.
After graduating from medical school in 2015, Graham completed her general surgical residency at the George Washington University in Washington, D.C., and her colorectal surgery fellowship at the University of Chicago.
She was drawn to colorectal surgery, she says, because she wanted opportunities to improve the quality of life for her patients. She also likes developing long-term relationships with her patients as well as the gastroenterologists who treat them, she says.
“With medicine and surgery, we have the possibility to make a pretty significant impact on a person’s life,” she says. “That’s what my job is, to get people back to doing the things that they want to be doing.”