Health care debt has become the leading contributor to individual bankruptcy and foreclosures in the United States. Both insured and uninsured patients are burdened by medical bills, and health care quality and safety are compromised as patients avoid necessary care.
These issues1 are the driving force behind the High Value Practice Academic Alliance, or HVPAA, a national consortium of more than 80 academic medical centers led by Johns Hopkins Medicine. The alliance held its inaugural research and education conference in Baltimore Oct. 8–9.
“Medical educators have an obligation to prepare the next generation of physicians to deliver high-value care,” said Roy Ziegelstein, vice dean for education at the Johns Hopkins University School of Medicine. “As a leader in both clinical care and medical education, Johns Hopkins must set the standard in this field.”
Nearly 200 clinicians, house staff members and administrators from 70 medical centers attended the conference, which featured innovative work from 50 institutions in the U.S. and Canada. Some 140 podium and poster presentations described quality-improvement projects that focused on delivering better patient care by reducing unnecessary health care practices.
“This is a new model for collaboration, one that transcends cross-institutional competition, geographic constraints and specialties,” said Pamela Johnson, vice chair of quality and safety in radiology at Johns Hopkins University School of Medicine, a co-founder of the HVPAA and organizer of the conference. “Academic medical centers have no choice but to step up to the plate, refine practice within their institutions and lead large scale improvement by disseminating results. We have to demonstrate to patients that we are accountable for delivering the improvements needed in the U.S. health care system.”
Breakthroughs and setbacks are both helpful
Through monthly calls, collaborative publications and multi-institution quality-improvement projects, HVPAA members share knowledge about both breakthroughs and setbacks in their efforts to eliminate unnecessary tests, procedures and treatments, and improve patient care.
“This conference is a testament to the fact that providers all over the country are thrilled to join together and share experiences, so that improvements can be advanced efficiently and effectively across the country,” said Johnson. “Medical centers are learning from each other and experienced centers are mentoring those new to high value care.”
Seth Martin, cardiologist and co-director of the Advanced Lipid Disorders Center at Johns Hopkins Medicine, echoed Johnson’s enthusiasm. “It can be validating to see that people are interested in what you are doing, but it can also stimulate questions that maybe you hadn’t thought about that can push your work further along,” said Martin, who was excited to share the advancements of the Corrie Health App, a mobile technology created by a team of Johns Hopkins clinicians and engineers that could improve patient recovery after a heart attack. “Interacting with peers at an innovative conference like this can really help round out your thinking.”
In the poster session, Claire Ciarkowski, a hospitalist in the division of general internal medicine at University of Utah Health Care, shared how her team had reduced lab utilization in the hospitalist service by 19 percent — without affecting length of stay or 30-day readmission rates.
“When we looked at the data nationally, we found that 30-50 percent of labs were unnecessary,” said Ciarkowski. “Patients get tests in the hospital almost every single day, and largely those tests are not going to impact the care they get that day and may actually cause other testing and variations of harm.”
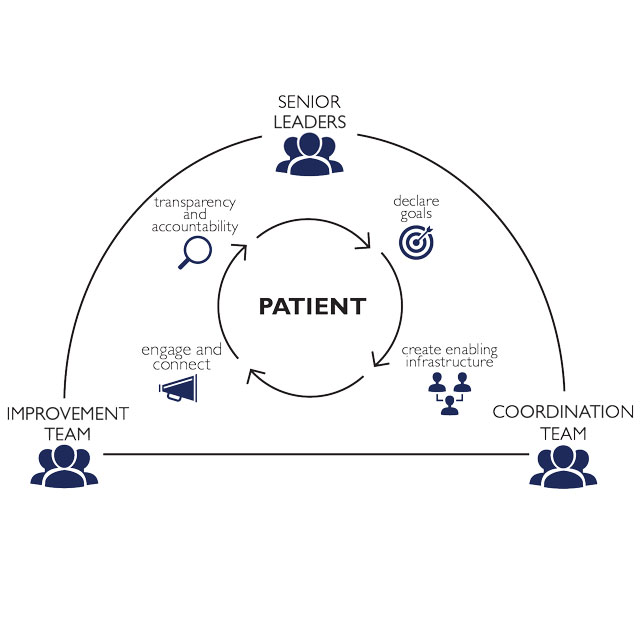
Indeed, reducing the chance of patient harm is an explicit goal of high-value medical practice. Peter Pronovost, senior vice president for patient safety and quality and director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins Medicine, spoke in his keynote address about the critical need to “change the narrative about patient safety.”
“For too long, we’ve accepted the narrative that patient harm is inevitable. But it’s not. Zero patient harm is an achievable goal, and one that we have a moral mandate to pursue,” said Pronovost. One of the founding principles of the HVPAA is to ensure that patient safety is not compromised by efforts to reduce unnecessary practice. The quality improvement abstracts at the conference included data about diagnosis and treatment efficacy.
Training the next generation of physicians is a priority for the HVPAA and was an important feature of the conference. The organization also directs a year-long high value care professional development program for 80 house staff members across the U.S.
“This is a really exciting time for academic health centers,” said Gulshan Sharma, vice president and chief medical and clinical innovation officer at The University of Texas Medical Branch. “We have mostly focused on education and research and now, more and more, we want to train our trainees in value-based care. This alliance is a great platform to combine all academic health centers so we can learn from each other and share best practices. Appropriateness in testing and treatment of patients is going to be key, regardless of the United States region where we practice.”
Pressures for improvement
In an effort to reduce wasteful spending and improve the patient experience, the Centers for Medicare and Medicaid Services will require all providers ordering radiological imaging tests to follow its appropriate-use criteria beginning January 2019.
“Providers who fail to follow the criteria will be identified and require preauthorization for future imaging orders,” Johnson told a packed room during a half-day continuing medical education session led by 15 Johns Hopkins radiology faculty members and aimed at teaching nonradiologists the appropriate guidelines for ordering tests.
Published data report that 20 to 50 percent of all imaging exams in the United States are unnecessary, said Johnson, and they bring associated risks related to radiation exposure and intravenous contrast, cause anxiety, waste time for patients and can result in incidental findings that precipitate even more unnecessary tests.
Elliot Fishman, director of diagnostic imaging and body computed tomography (CT) at Johns Hopkins Medicine, shared findings from a 2011 study conducted by himself; Johnson; Karen Horton, director of radiology at Johns Hopkins; and others. The study showed wide disagreement among radiologists on interpreting incidental findings on CT.
“Of the 12 most common incidental findings, we only found a 70 percent or greater agreement on interpretation for six findings,” said Fishman. “This was both within departments and across institutions.” The good news, he says, is that education makes an impact.
In 2014, the Journal of the American College of Radiology reported on a survey that showed 560 radiologists (51 percent of the sampling) who had read a white paper from the American College of Radiology Incidental Findings Committee were less likely to recommend more imaging, while only 33 radiologists (3 percent of the sampling) were likely to recommend imaging more often when reviewing incidental findings.
The Johns Hopkins radiology team is developing a “when and what to order” pocket guide to place in white coats to help providers order the appropriate imaging tests. The guide, which is expected to be published by the end of 2017, will be available in print for Johns Hopkins Medicine staff members. Outside providers will be able to download the guide for free online. Download the demo now at orderwisely.org.
Learn more about the HPVAA at hvpaa.org.