-
Jee Bang, M.D., M.P.H.
- Clinical Director, Johns Hopkins Huntington Disease Center of Excellence
- Assistant Professor of Neurology
- Assistant Professor of Psychiatry and Behavioral Sciences
-
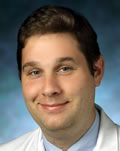
Ankur Ajit Butala, M.D.

- Assistant Professor of Neurology
- Assistant Professor of Psychiatry and Behavioral Sciences
-
Kelly Mills, M.D., M.H.S.

- Director, Movement Disorders Division
- Director, Neuromodulation and Advanced Therapies Clinic
- Associate Professor of Neurology
-
Alexander Pantelyat, M.D.
- Director, Atypical Parkinsonism Center
- Co-Founder and Co-Director, Johns Hopkins Center for Music & Medicine
- Co-Director, Johns Hopkins Movement Disorders Fellowship
- Associate Professor of Neurology
The Johns Hopkins Movement Disorders Fellowship

The Johns Hopkins Movement Disorders fellowship aims to train exceptionally qualified individuals in the diagnosis and management of a wide variety of movement disorders, as well as provides scholarly training in conducting movement disorders research.
On this page: Rotations | Directors | Specialty Centers | Faculty | Fellows | Alumni
Program Overview

- Duration: 2-3 years
- Program start: July
- Eligibility: by the start of the fellowship training, candidates must have completed an ACGME-accredited residency program in neurology and are board-certified or board-eligible.
- How to apply: Applications are accepted through the SF Match portal. Please submit your CV, medical school transcripts and three letters of recommendation (letter from residency director or departmental chairman strongly recommended).
Program Directors
The Division Director and Director of the Fellowship Training Program review applications and invite selected candidates for an interview. For more information, please contact:
Alexander Pantelyat, M.D.
Assistant Professor of Neurology
The Johns Hopkins Hospital, Meyer 6-181C
600 N. Wolfe Street
Baltimore, MD 21287
410-502-3290 (tel)
410-502-6737 (fax)
[email protected]
Jee Bang, MD
Assistant Professor of Neurology
The Johns Hopkins Hospital, Meyer 6-181E
600 N. Wolfe Street
Baltimore, MD 21287
410-502-4125 (tel)
410-502-6737 (fax)?
[email protected]
Rotations and Responsibilities
The fellowship curriculum involves structured rotations through subspecialty clinics. The program’s close relationship with other departments ensures exposure to pediatric neurology, neuro-ophthalmology, neuropsychiatry, cognitive neurology, adult hydrocephalus and telemedicine.
- The first year of fellowship is clinically intensive, intended to give junior fellows a well-rounded experience in the evaluation and management of movement disorders and build a robust clinical understanding of various phenomenologies and disease processes. Clinic time is split among attending clinics, neuromodulation, chemodenervation, ataxia and fellows' continuity clinics.
- In the second year, fellows are encouraged to tailor their clinical experience based on post-fellowship career goals while building on their first year foundation. The inpatient movement disorders consult coverage is divided among the first- and second-year fellows.
-
Movement disorders consult requests from the Johns Hopkins Hospital (main campus) are handled by the inpatient movement disorders consult service comprising one fellow and one staffing attending on a monthly rotation. The consult coverage is provided for weekdays only. This is intended to provide experience with emergencies in movement disorders, acute movement disorders presentations and evaluating patients in an inpatient setting. The consult volume ranges from 0-10 consults per month, with an average of 4 - 6.
-
Fellows are expected to develop their own research projects or take leadership roles in one or more projects in development. Options include projects under the Udall Center of Excellence, Huntington's Disease Center, Atypical Parkinsonism Clinic, Neuromodulation Center, The Institute of Cell Engineering and Ataxia Center.
Fellows are also encouraged to seek out projects from outside the division in areas such as radiology, neuroimmunology, pediatric neurology and psychiatry. The department of Neurology provides support for writing grants (internal grant review) and critical appraisal of projects. Biostatistical and research project support are provided through the Johns Hopkins Institute for Clinical and Translational Research.
-
The division facilitates several patient support activities through its community outreach programs, patient-caregiver engagement events and fundraisers. Our fellows can lend their expertise through public lectures and informational articles on research in newsletters and other media. These activities foster fellows' experience in community outreach, public engagement in research and future practice development.
As a referral center for many international patients, Johns Hopkins offers unique opportunities to interact with patients and their local providers from diverse backgrounds. This includes the option to participate in telemedicine initiatives in movement disorders.

-
Numerous intramural conferences under the umbrella of Johns Hopkins' departments of Neurology and Psychiatry are available to the fellows for expanding their medical education. Movement disorders fellows are expected to prepare and present topics, cases and videos for the following meetings in rotation.
- Johns Hopkins Topic Discussion for Movement Disorders Fellows (JHoT): First and third Wednesdays. Topics cover the breadth of movement disorders, divided among attendings and fellows
- Movement Disorders Video Case Conference: Third Wednesdays (following JHoT). Discussion of teaching cases and those needing consensus
- Ataxia Center Meeting: Second Fridays. Various ataxia topics
- Neuromodulation and Advanced Therapies Committee Meeting: Second Wednesdays. Fellow-run conference, presentation and discussion of candidates for advanced therapies
- Tauopathy Consensus Conference: Fourth Tuesdays. Consensus diagnosis of tauopathy subtypes
- Neurology Grand Rounds: Thursdays
The Maryland-Washington Regional Movement Disorders Video Meeting is a regional quarterly meeting cohosted by the movement disorders divisions at the NIH, University of Maryland, Georgetown University, Walter Reed and Johns Hopkins attended by academic and private community neurologists. The congress typically hosts a guest speaker or a speaker from the respective hosting academic institution, followed by a collegial video conference session.
The incoming fellows are strongly encouraged to attend the "Aspen Conference" organized by the International Parkinson’s and Movement Disorders Society (MDS). Opportunities to attend various conferences organized by the foundations for Parkinson's disease, ataxia, atypical Parkinsonian disorders and HD are also available.
Subspecialty Clinics and Centers
Our diverse faculty includes experts from several divisions and departments, who are dedicated to teaching fellows and ensuring a well-rounded clinical experience with common and rare movement disorders. Our multidisciplinary care, involving the allied health team and experts in genetics, neuromodulation and chemodenervation provides a comprehensive approach to complex movement disorders and encourages team building, which is critical for modern clinical practice.?
-
The Parkinson's Disease and Movement Disorders Center at Johns Hopkins University School of Medicine, which is a Parkinson’s Foundation Center of Excellence, provides comprehensive care to a large patient demographic, including local, national and international patients. Fellows rotate with attendings in general movement clinics as well as subspecialty clinics. Fellows also follow patients longitudinally in botulinum toxin and general movement disorders continuity clinics over the course of their two-year fellowship.
-
The selection of patients for deep brain stimulation (DBS) surgery, intrajejunal levodopa infusion therapy, and other advanced therapies is performed through the neuromodulation and advanced treatments center. Patients are evaluated and video-recorded by fellows in their medication ON and OFF states and discussed at the Multidisciplinary Neuromodulation and Advanced Treatments (NeuModAT) committee meeting. Fellows also work with neuropsychology and psychiatry in patient selection and follow-up of neurocognitive and neuropsychiatric outcomes. Continuity of care is encouraged so that fellows may follow patients from their preoperative evaluation to their OR day and subsequent DBS programming.
-
A wide range of primary and secondary dystonias of varying complexity are treated with a variety of botulinum toxins under EMG and ultrasound guide at the chemodenervation clinics under the division. Fellows have monthly injection clinics supervised by attendings. Additionally, fellows rotate through attending-run clinics. Physical medicine department also runs chemodenervation clinics where fellows can arrange rotations. Our fellows also may shadow experts at the NIH at the Bethesda campus.
-
The Johns Hopkins Ataxia Center caters to a large and diverse group of ataxic and spastic patients with inherited and acquired disorders such as spinocerebellar ataxias, Friedrich ataxia, mitochondrial disorders, hereditary spastic paraparesis, episodic ataxias, and idiopathic ataxia. The Ataxia Clinic utilizes a multidisciplinary team-based approach to patient care, and fellows have the opportunity to rotate with the genetic counselor, PT, OT, and SLP as they evaluate and treat patients. Close collaboration with neuro-visual and vestibular specialists also ensures exposure to a variety of eye movement and vestibular pathologies.
-
Since 2014, Johns Hopkins has served as a primary referral center for all atypical Parkinsonian syndromes, including progressive supranuclear palsy (PSP), corticobasal degeneration (CBD), dementia with Lewy bodies (DLB), and multiple system atrophy (MSA). The Atypical Parkinsonism Center has been designated as a CurePSP Center of Care and Lewy Body Dementia Association Research Center of Excellence. There is a monthly multidisciplinary clinic for patients with atypical Parkinsonism, during which patients have the opportunity to meet with social work, physical/occupational/speech/swallow therapists, and discuss research opportunities. Additional clinics for frontotemporal dementia (FTD), memory disorders, and adult hydrocephalus are available for interested fellows.
-
The Johns Hopkins Huntington Disease Center is one of the pioneers in early identification and characterization of the phenotypes of Huntington and related disorders. Founded in 1980, the Center represents a unique partnership between the neurology and psychiatry departments and is a longstanding Huntington Disease Society of America (HDSA) Center of Excellence. In the HD clinic, we provide multidisciplinary clinical services including genetic counseling and social work support to individuals with HD and related disorders. Fellows rotate through the clinic to gain experience in the diagnosis and management of patients with HD and HD-like disorders. The center is involved in many multicenter clinical trials, often via the Huntington Study Group (HSG). It is currently the top site in the US for the CSF biomarker trial (“HDClarity”), and is poised to be a leading site for upcoming disease-modifying therapy trials employing involving strategies like antisense oligonucleotides (ASO).
-
Pediatric general movement disorders and pediatric ataxia clinic are available for our fellows. This includes a subspecialty Tic Tourette syndrome and stereotypy clinic which fellows can work in. Additional subspecialty rotations are also available through pediatric neurology clinics and the Kennedy Krieger Institute for interested fellows.
-
The various centers in the Movement Disorders division collaborate with genetics clinics to provide genetic counseling and testing for patients. Fellows work closely with our geneticists to gain insights into patient selection for genetic testing, genetic and reproductive counseling, and appropriate options for testing.
-
The multidisciplinary Ataxia and Atypical Parkinsonism clinics offer clinicians the opportunity to work closely with experts in physical therapy, occupational therapy and speech-language pathology. Additional experience with special patient populations is available through the PM&R department.
Core Fellowship Faculty
Other Faculty Educators
-
Argye Hillis, M.D.

- Director, Center of Excellence in Stroke Detection and Diagnosis, Sheikh Khalifa Stroke Institute
- Sheikh Khalifa Stroke Institute Professor of Acute Stroke Diagnoses and Management
- Director, Cerebrovascular Division of Neurology
- Executive Vice Chair, Department of Neurology
- Professor of Neurology
- Professor of Physical Medicine and Rehabilitation
-
Chiadi Onyike, M.B.B.S., M.D.
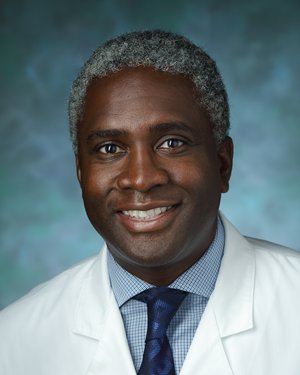
- Director, Frontotemporal Dementias Program
- Director, Young-Onset Dementias Program
- Associate Professor of Psychiatry and Behavioral Sciences
-
David Zee, M.D.
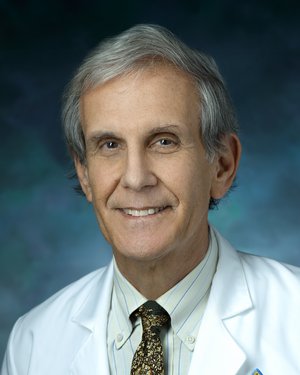
- Professor of Neurology
- Professor of Neuroscience
- Professor of Ophthalmology
- Professor of Otolaryngology - Head and Neck Surgery
Current Fellows
Stephen Berger, MD | Class of 2024
Medical School: New York University (2018) Residency: New York University (2018-2022)
Joseph Seemiller, MD | Class of 2024
Medical School: Geisinger Commonwealth University (2018)
Residency: Geisinger Health System (2018-2022)

Lauryn Currens, MD | Class of 2025
Medical School: St. George’s University School of Medicine (2019)
Residency: University of Massachusetts (2023)

Fellowship Alumni
Nigel Harrison, MD | 2023
Current Position: Intermountain Healthcare
Ashley Paul, MD | 2022
Current Position: Faculty, Johns Hopkins University
Maitreyi Murthy, MBBS | 2021
Current Position: Staff, PeaceHealth, Vancouver, WA
Jumana Alshaikh, MBBS |2021
Current Position: Faculty, University of Utah
Gerson Suarez-Cedeno, MD | 2020
Current Position: Unknown
Bonnie Kaas, MD | 2019
Current Position: Staff, Sinai Hospital of Baltimore
Suraj Rajan, MD | 2019
Current Position: Staff, OhioHealth Physicians Group
Ankur Butala, MD | 2018
Current Position: Faculty, Johns Hopkins University
Emile Moukheiber. MD | 2018
Current Position: Faculty, Johns Hopkins University
Martin Kronenbuerger, MD | 2017
Current Position: Unknown
Laura Tochen, MD | 2016
Current Position: Staff, Children's National Hospital
Chizoba Umeh, MD | 2013
Current Position: Faculty, Tufts University
Liana Rosenthal, MD | 2012
Current Position: Faculty, Johns Hopkins University
Shawn Smyth, MD | 2011
Current Position: Private Practice
Rainer von Coelln, MD | 2010
Current Position: Faculty, University of Maryland
Joseph Savitt, MD, PhD | 2003
Current Position: Faculty, University of Maryland
Michael Cooper, MD | 1999
Current Position: Faculty, Vanderbilt University
Allen Mandir, MD, PhD | 1998
Current Position: Faculty, Georgetown University
Ted M. Dawson, MD, PhD | 1992
Current Position: Professor, Johns Hopkins University
Jerrold Vitek, MD, PhD | 1990
Current Position: Professor, University of Minnesota
Steven Reich, MD | 1988
Current Position: Professor, University of Maryland