Left Atrial Appendage Closure Procedures
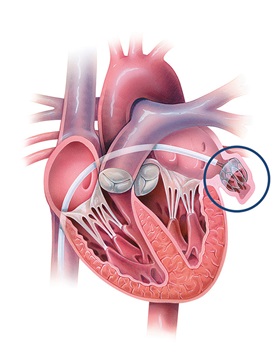
Stroke is a serious risk for patients with atrial fibrillation, which is caused by a disruption of electrical signals in the muscles of the upper chambers of the heart. When the heart pumps in an irregular, uncoordinated way, there is a decreased flow of blood to the body, which is typically slow moving and likely to cause a blood clot. In the majority of cases, the clots form in the left atrial appendage, a small, pouchlike sac in the top left chamber of the heart. If the clots travel through the arteries in the heart, they can cause a stroke.
If you are a patient with atrial fibrillation who is at increased stroke risk, your doctor will recommend that you be placed on a blood thinner. If you are unable to take a blood thinner because of risk of bleeding or falls, your doctor may recommend a procedure to occlude your left atrial appendage.
Atrial Fibrillation (AFib) | Q&A with Dr. Hugh Calkins
Catheter-Inserted Closure Devices
WATCHMAN™ Device
One procedure used to close the left atrial appendage is a self-expanding, parachute-shaped device with an attached woven plastic cap called the WATCHMAN™ device. This device is approved by the FDA to reduce the risk of thromboembolism from the left atrial appendage in patients with nonvalvular atrial fibrillation who are not good candidates for long-term anti-coagulation.
The Procedure
The procedure is performed under general anesthesia. The physician inserts the delivery catheter into the body through a vein in the leg. The catheter is advanced through the bloodstream until it reaches the upper right chamber of the heart. The physician makes a small hole through the wall between the two upper chambers of the heart so that the catheter reaches the left atrium. The physician then pushes the device through the delivery catheter into the left atrial appendage, where it opens up like an umbrella and is permanently implanted. Once the device is in place, a thin layer of tissue grows over it in about 45 days. This keeps blood clots in the left atrial appendage from entering the bloodstream.
What are the risks?
Although the device is a permanent solution, there is a small incidence of complications associated with the implantation procedure. Your doctor can go over the risks and benefits of this procedure with you in detail.
What happens after the procedure?
-
You will have a follow-up appointment 45 days after the procedure. At that point your, anti-coagulant medication will be stopped if complete occlusion of the left atrial appendage is demonstrated.
-
Once the left atrial appendage is blocked, you will remain on low-dose aspirin indefinitely.
LARIAT Device
The Procedure
The second catheter-based procedure uses a device called LARIAT to place a loop stitch around the base of the left atrial appendage, permanently sealing it off from the rest of the heart and blocking stroke-causing blood clots from entering the brain. Johns Hopkins is currently the only center in the mid-Atlantic region offering LARIAT as an option. Patients who have had prior cardiac surgery are not candidates for this procedure. A CT scan will need to be performed to make certain that the left atrial appendage is not too large or has an unusual location that precludes placement of this device.
What are the risks?
The use of the suture delivery device does not require the use of immediate use of blood thinners. As with any invasive procedure, there are risks to placement of this type of device. Your doctor can go over these risks in detail.
What happens after the procedure?
-
You will have a follow-up appointment 45 days after the procedure.
-
Once the left atrial appendage is blocked, you will be followed on a routine basis by your referring physician.
ArtiClip Device
The Procedure
The AtriClip, which is applied to the outside surface of the left atrial appendage, permanently closes the left atrial appendage at its base, preventing blood from entering the pouch. This procedure is performed by a cardiac surgeon using minimally invasive surgical techniques. You do not need to be on a blood thinner before or after this procedure.
What happens after the procedure?
-
You will have a follow-up appointment 45 days after the procedure.
The Johns Hopkins Heart and Vascular Institute: An Overview
Cardiologists, cardiac surgeons and vascular specialists work together to lead the way in cardiovascular disease prevention and treatment through research and clinical care.







