Endovascular Coiling
What is endovascular coiling?
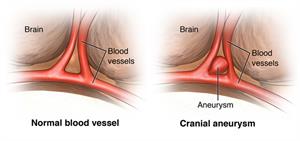
Healthcare providers use endovascular coiling to block blood flow into an aneurysm. This procedure is also called endovascular embolization. An aneurysm is a weakened area in the wall of an artery. If an aneurysm breaks open (ruptures), it can cause life-threatening bleeding and brain damage. Preventing blood flow into an aneurysm helps to keep it from rupturing.
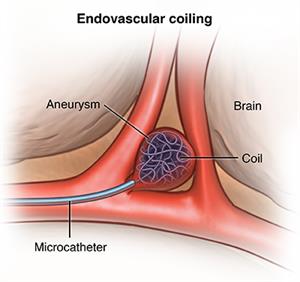
For endovascular coiling, the healthcare provider puts a long, thin tube (catheter) into a groin artery. The healthcare provider moves the catheter into the affected brain artery and puts the coil in place. X-rays help guide the catheter into the artery. The coils are made of soft platinum metal and are shaped like a spring. The coils are very small and thin. They range in size from about twice the width of a human hair to less than one hair's width. Sometimes coils are used with stents to prevent the coils from moving out of the aneurysm.
Healthcare providers also use coiling to treat a condition called arteriovenous malformation (AVM). An AVM is a tangling of blood vessels that cause an abnormal link between an artery and a vein. It may happen in the brain, spinal cord, or elsewhere in the body.
Why might I need endovascular coiling?
Healthcare providers mainly use coiling to treat a cerebral aneurysm at risk for rupturing. In some cases, they may use it to fix a ruptured aneurysm.
There may be other reasons for your healthcare provider to advise a coiling procedure.
What are the risks of endovascular coiling?
If you are pregnant or think you may be pregnant, tell your healthcare provider.
There is a risk for allergic reaction to the dye that's used to see the aneurysm on an X-ray. Tell the radiologist or technologist if you are allergic to or sensitive to medicines, contrast dye, or iodine. Also tell the radiologist if you have kidney failure or other kidney problems.
Also tell your healthcare provider if you take anticoagulant (blood-thinning) medicines such as aspirin, warfarin, or clopidogrel. You may need to stop taking these medicines for 1 or more days before the procedure to prevent bleeding.
Because the procedure involves the blood vessels and blood flow of the brain, there is a risk for complications involving the brain. These complications may include:
-
The coils poking through the aneurysm or a blood vessel
-
Loss of consciousness
-
Stroke or mini-stroke (transient ischemic attack). This can be from a blood clot or a coil moving into the wrong artery.
-
Paralysis of one-half of the body
-
Blood clot
-
Bleeding
-
Area of swelling caused by a collection of blood (hematoma)
-
Loss of the ability to speak or understand speech (aphasia)
-
Infection
-
Rupture of aneurysm
-
Higher chance of an aneurysm returning
-
Blood collection (hematoma) in your groin, where the catheter was inserted
You may have other risks depending on your specific health condition. Discuss any concerns with your healthcare provider before the procedure.
How do I get ready for an endovascular coiling?
-
Your healthcare provider will tell you about the procedure and offer you a chance to ask any questions.
-
You will be asked to sign a consent form that gives permission to do the procedure. Read the form carefully and ask questions if something is not clear.
-
Tell your healthcare provider if you have ever had a reaction to any contrast dye or if you are allergic to iodine.
-
Tell your healthcare provider if you are sensitive to or are allergic to any medicines, latex, tape, or anesthetic medicines (local and general).
-
Follow any directions you are given for not eating or drinking before surgery.
-
Tell your healthcare provider if you are pregnant or think you may be pregnant.
-
Tell your healthcare provider about all the prescription and over-the-counter medicines and herbal supplements that you are taking.
-
Tell your healthcare provider if you have a history of bleeding disorders. Also tell your healthcare provider if you are taking any anticoagulant (blood-thinning) medicines, aspirin, or other medicines that affect blood clotting. You may need to stop taking these medicines before the procedure.
-
Your healthcare provider may order a blood test before the procedure to find out how long it takes your blood to clot. Other blood tests may be done as well.
-
Based on your health condition, your healthcare provider may give you other instructions.
What happens during an endovascular coiling?
You will need to stay in the hospital for a coiling procedure. Procedures may vary depending on your condition and your healthcare provider's practices.
Your procedure may be done by one or both of these specialists:
-
Neurosurgeon. This healthcare provider specializes in surgery and treatment of the nervous system.
-
Interventional radiologist. This healthcare provider specializes in diagnostic and treatment methods using radiology techniques.
During the procedure, you are asleep under general anesthesia. In some situations, it may be done under local anesthesia.
Generally, a coiling procedure follows this process:
-
You will be asked to remove any clothing, jewelry, hairpins, dentures, or other objects that may interfere with the procedure. You will be given a hospital gown to wear.
-
You will be given time to empty your bladder before the start of the procedure.
-
You will be positioned on your back on the X-ray table.
-
An IV (intravenous) line will be started in your hand or arm.
-
You will be connected to an electrocardiogram (ECG) monitor that records the electrical activity of the heart. Your heart rate, blood pressure, breathing rate, and nervous system signs will be monitored during the procedure.
-
A catheter may be put into your bladder to drain urine.
-
The radiologist or neurosurgeon will check your pulses below the groin site where the catheter will be inserted. The healthcare provider will mark them with a marker so that the circulation to the limb below the site can be checked after the procedure.
-
The healthcare team will clean the skin over the injection site. You will be given a local anesthetic.
-
The radiologist or neurosurgeon will make a small cut (incision) in the skin to expose the artery in the groin.
-
The healthcare provider will put a catheter into the artery in your groin using a guide wire. The catheter will be guided through the blood vessel into the brain using fluoroscopy. This is a special type of X-ray, similar to an X-ray "movie."
-
Once the catheter reaches the affected artery in the brain, contrast dye will be injected to make the aneurysm and surrounding blood vessels visible on X-ray.
-
The healthcare provider will measure the aneurysm and record its shape and other aspects.
-
The healthcare provider will put a smaller catheter into the initial catheter.
-
Once the catheter has reached the aneurysm, the healthcare provider will move the coil into the aneurysm.
-
When the coil has been completely placed into the aneurysm, the coil is released from the catheter.
-
The healthcare provider will put in as many coils as needed to completely seal off the aneurysm. The coils will form a mesh-like structure inside the aneurysm.
-
After the aneurysm has been "packed" with coils, more X-ray images will be taken to make sure the aneurysm has been sealed off. The coil is left in place in the aneurysm.
-
Once the aneurysm has been sealed off, the catheter will be removed. After the insertion site stops bleeding, a dressing will be applied.
What happens after an endovascular coiling?
In the hospital
After the procedure, you may be taken to the recovery room or the ICU (intensive care unit) for observation. If the coiling procedure was done for a ruptured aneurysm, you will most likely be taken to the ICU. If the coiling procedure was done for an unruptured aneurysm and your condition is otherwise stable, you may be able to go home a day or two after the procedure.
You will remain flat in bed for as long as 12 to 24 hours after the procedure. A nurse will monitor your vital signs, nervous system signs, the insertion site, and circulation or sensation in the affected leg.
You may be given pain medicine for pain or discomfort from the procedure or from having to lie flat and still for a long period.
You may go back to your usual diet after the procedure unless your healthcare provider tells you otherwise.
Once you have recovered, you may be able to go home, unless your healthcare provider decides otherwise. In some cases after repair for a ruptured aneurysm, you may need to stay at a rehab facility. This is to help you recover from damage caused by the ruptured aneurysm.
At home
You may be advised not to do any strenuous activities. Your healthcare provider will tell you when you can return to work and go back to your normal activities. Tell your healthcare provider if you have any of the following:
-
Fever or chills
-
Increased pain, redness, swelling, or bleeding or other drainage from the insertion site
-
Coolness, numbness or tingling, or other changes in the affected leg
-
Any changes in bodily functions or your nervous system, such as a very bad headache, seizure, or loss of consciousness
Generally, you will need to schedule follow-up cerebral angiograms after the procedure. This test is done to make sure the coiling is working. The first angiogram may be done about 1 month after the procedure. You may have other cerebral angiograms or other imaging tests such as MRI or MRA. Your healthcare provider will let you know how often you need these.
Your healthcare provider may give you other instructions about what you should do after an endovascular coiling.
Next steps
Before you agree to the test or the procedure, make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you will get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you will have to pay for the test or procedure


