Hypertrophic Cardiomyopathy
What is hypertrophic cardiomyopathy?
Hypertrophic cardiomyopathy, or HCM, is a disease that causes thickening (hypertrophy) of the heart muscle. The heart muscle cells enlarge more than they should and scarring often develops between the cells.
The left and right ventricles are the 2 lower chambers of the heart. A muscular wall called the septum separates these 2 ventricles. With HCM, the walls of the ventricles and septum may thicken abnormally.
The thickened septum may bulge into the left ventricle and partially block the blood flow out to the body. This is called obstructive hypertrophic cardiomyopathy. When this happens, the heart must work harder to get the blood out to the body.
Because of thickened heart muscle, the inside of the left ventricle is smaller, so it holds less blood than normal. The ventricle can also become very stiff. As a result, it is less able to relax and fill with blood.
HCM can also damage the mitral valve, which can increase pressure in the ventricles. This can cause fluid to build up in the lungs. The abnormal heart cells in HCM can also set off abnormal heart rhythms.
HCM is a common condition. It affects the same numbers of men and women. In most cases, the symptoms first appear during adolescence or young adulthood.
What causes hypertrophic cardiomyopathy?
HCM is a genetic problem that you inherit from your parents. It leads to the thickening of the left ventricle. How exactly this happens is not yet clear.
HCM is autosomal dominant. This means you need an abnormal gene from only one of your parents to have it. But even if you have an abnormal gene, you might not develop HCM. Researchers are still trying to understand what other factors increase the chances of having the disease.
Who is at risk for hypertrophic cardiomyopathy?
Having a first degree relative with HCM puts you at risk for the disease. A parent with an abnormal gene for this condition, has a 50% chance of giving that gene to a child. If someone in your immediate family has HCM, specific screening protocols should be followed. Screening typically includes a history, physical exam, electrocardiogram (ECG) and an echocardiogram. Genetic testing is available, but this is not routinely recommended for screening and diagnosis.
What are the symptoms of hypertrophic cardiomyopathy?
Most people with HCM have few or no symptoms. Symptoms most commonly appear during adolescence or young adulthood. The onset and severity of symptoms varies among those with the condition. These may include:
- Shortness of breath with activity
- Shortness of breath when lying flat
- Chest pain, especially with activity
- Fainting or near fainting
- Unpleasant awareness of the heartbeat (palpitations)
- Fatigue
- Swelling in the legs and feet
- Abnormal heart rhythms
How is hypertrophic cardiomyopathy diagnosed?
Your healthcare provider will take your medical history and do a physical exam, noting any heart murmurs. Several tests may also help in the diagnosis. These tests include:
- Electrocardiogram (ECG). This test is done to look for abnormalities in heart rhythm.
- Echocardiogram (ECHO). This test can confirm the diagnosis. Echocardiogram will provide more detailed information about the heart’s structure and function.
- Stress echocardiogram (ECHO). This test involves exercising on a treadmill or stationary bike with an echocardiogram. This examines the heart's response to exertion in detail.
- Continuous portable electrocardiogram monitoring. This is a portable ECG that can record abnormal heart rhythms throughout the day.
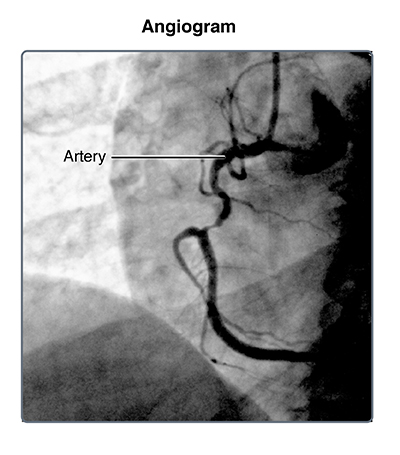
- Other tests. These may include MRI of the heart, cardiac catheterization, or coronary angiography (less common).
- Genetic testing. In rare cases, your healthcare provider may do genetic testing.
If a person has HCM, other members of the family should be tested. This includes all the siblings, parents, and children of the person diagnosed with the disease.
How is hypertrophic cardiomyopathy treated?
Treatment for HCM aims to decrease symptoms and the chance of complications. The best treatment for you will depend on your specific symptoms. Some general types of treatment include:
- Activity restriction: talk to your healthcare provider about what kinds of exercise you can do. You may need to avoid most competitive sports. You may also need to avoid isometric exercise (like weight lifting) and burst exercise (like sprinting).
- Avoiding dehydration
- Medicines to treat shortness of breath and chest pain: some examples include beta-blockers and calcium-channel blockers. These drugs help improve blood flow to the heart, and decrease the heart’s need for oxygen. They will improve the heart’s ability to fill with blood and decrease the obstruction of blood flow to the body.
- Medicines to help prevent abnormal heart rhythms: these help to change the electrical activity in the heart.
- Anticoagulants: these are also called blood thinners. They include medicines such as warfarin. These are used if you have certain abnormal heart rhythms. This reduces the risk of stroke.
- Septal myectomy: this is surgery to remove a portion of the septal wall so more blood can fill the ventricle and be pumped out to the body.
- Alcohol septal ablation: in this procedure, pure alcohol is injected into certain blood vessels to destroy the segment of muscle that is blocking blood flow out of the heart.
- Implantable cardioverter defibrillator (ICD). This implanted device monitors for dangerous heart rhythms and can restore normal rhythm with an energy shock. It is placed in people who are at a particularly high risk of dangerous heart rhythm and cardiac arrest.
Septal myectomy and alcohol septal ablation may be done in people with severe symptoms or complications that do not improve with medicines. Both procedures help blood exit the left ventricle more easily.
What are the complications of hypertrophic cardiomyopathy?
Most people with HCM do not have complications. But some do, especially if their disease is more severe. These complications may include:
- Heart failure
- Stroke
- Abnormal heart rhythms
- Infection of the heart valves (endocarditis)
- Increased risk of complications during pregnancy
- Sudden cardiac death (from a dangerous heart rhythm)
Sudden death is rare in people with HCM. If you are at risk for sudden death, your healthcare provider may recommend an implantable cardioverter-defibrillator (ICD).
How do I manage hypertrophic cardiomyopathy?
Your healthcare provider may give you additional instructions about how to manage your HCM.
- You may need to avoid certain drugs that can make your HCM worse. These include drugs like ACE inhibitors and certain drugs for erectile dysfunction.
- Work closely with your healthcare provider if you are planning to become pregnant.
- Your healthcare provider may want to treat you for other heart conditions. This might include medicines for high cholesterol.
- Your healthcare provider might recommend other lifestyle changes, like losing weight, quitting smoking, or improving your diet.
- You may need to reduce your intake of alcohol or caffeine. (These increase the risk of abnormal heart rhythms.)
When should I call my healthcare provider?
See a healthcare provider right away if you have severe symptoms like chest pain, passing out, or severe shortness of breath. If your symptoms are gradually increasing, plan to see your healthcare provider soon. Make sure all of your healthcare providers know about your medical history.
Key points
HCM causes abnormal growth of the heart muscle. Most people with HCM have few or no symptoms. Most lead long lives. But HCM sometimes causes serious complications, including sudden cardiac death.
- Follow your healthcare provider’s instructions carefully. Follow any exercise precautions given. Take all your medicine as prescribed.
- If you have HCM, see your healthcare provider regularly for monitoring. This is important even if you do not have any symptoms.
- Most people with HCM do not require extensive treatment, although regular monitoring is important. Some people need medicines or surgical procedures.
- Tell your healthcare provider if you have severe symptoms or if your symptoms increase.
- Other family members may require assessment for HCM.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.