Heart Block
What is heart block?
Electrical signals control the beating of your heart. They tell your heart muscle when to contract, a process known as conduction. The normal timing of heartbeats is generated in the upper chamber of the heart (atria) in a structure called the sinus node. When you have heart block, there is interference with the electrical signals that usually move from the atria to the ventricles. These signals tell your heart when to beat. This is known as a conduction disorder. If the electrical signals can’t move from your atria to your ventricles, they can’t tell your ventricles to contract and pump blood correctly.
In most cases of heart block, the signals slow down, but do not completely stop. Heart block is categorized as first-, second-, or third-degree:
- First-degree heart block is the least severe. The electrical signals slow down as they move from your atria to your ventricles. First-degree heart block might not require treatment of any kind.
- Second-degree heart block means that the electrical signals between your atria and ventricles can intermittently fail to conduct. There are 2 types of second-degree heart block
- Mobitz type I: The electrical signals get slower and slower between beats. Eventually your heart skips a beat.
- Mobitz type II: The electrical signals sometimes get to the ventricles, and sometimes they do not. There is no progressive slowing of the electrical signal. This type of heart block can often progress to third degree heart block.
- Third-degree heart block is the most severe. Electrical signals do not go from your atria to your ventricles at all with this type. There is a complete failure of electrical conduction. This can result in no pulse or a very slow pulse if a back up heart rate is present.
What causes heart block?
If you are born with heart block, you have congenital heart block. Either a condition your mother had during her pregnancy, or heart problems you were born with, cause this condition.
For most, heart block develops as you get older as the wires that connect the top and bottom of the heart can develop fibrosis and eventually fail. Sometimes this may happen due to advancing age. Any process which can damage these heart wires can result in heart block.
Coronary artery disease with and without a heart attack is one of the most common causes of heart block. Cardiomyopathies which are diseases that weaken the heart muscle can also result in wire damage. Any disease that can infiltrate the heart such as sarcoidosis and certain cancers or any disease that results in heart inflammation such as certain autoimmune disease or infections can result in heart block. Electrolyte abnormalities especially high potassium levels can also result in wire failure.
Who is at risk for heart block?
If you are born with heart block, you have congenital heart block. Either a condition your mother had during her pregnancy, or heart problems you were born with, cause this condition. Many instances of heart block occur because of some other condition or event such as:
- Older age
- Heart attack or coronary artery disease
- Cardiomyopathy
- Sarcoidosis
- Lyme disease
- High potassium levels
- Severe hyperthyroidism
- Certain hereditary neuromuscular diseases
- Medicines that slow the heart rate
- Post open heart surgery
What are the symptoms of heart block?
Symptoms depend on the type of heart block you have:
First-degree heart block may have no bothersome symptoms.
- Dizziness
- Fainting
- The feeling that your heart skips beats
- Chest pain
- Trouble breathing or shortness of breath
- Nausea
- Fatigue
Third-degree heart block, which can be fatal, might cause
- Intense tiredness
- Irregular heartbeats
- Dizziness
- Fainting
- Cardiac arrest
How is heart block diagnosed?
To diagnose your condition, your healthcare provider will consider:
- Your overall health and medical history
- Any family history of heart block or heart disease
- Medicines you are taking
- Lifestyle choices, such as use of cigarettes or illegal drugs
- Your description of symptoms
- A physical exam
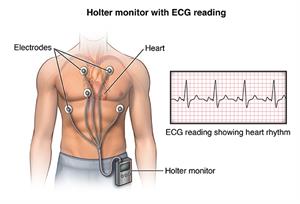
- An electrocardiogram (ECG) that records your heart’s electrical impulses
- Testing with a Holter or event monitor to track your heart’s rhythm for a period of time. You might wear a Holter monitor for 24 or 48 hours, or an event monitor for a month or more. These help capture changes in your heart’s rhythm, even if they do not occur often or predictably.
- Implantable loop recorder, a small heart recorder that is placed underneath the skin overlying the heart that can record up to 2 years duration.
- An electrophysiology study, which is an outpatient procedure in which a thin, flexible wire is threaded from your groin or arm to your heart to test the heart's wiring system.
How is heart block treated?
You treatment depends on the type of heart block you have:
- With first-degree heart block, you might not need treatment.
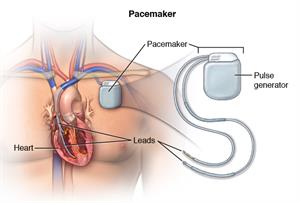
- With second-degree heart block, you may need a pacemaker if symptoms are present or if Mobitz II heart block is seen.
- With third-degree heart block, you will most likely need a pacemaker.
In addition, your medical team may make changes in any medicines you're taking.
What are the complications of heart block?
With heart block, complications may include fainting with injury, low blood pressure, and damage to other internal organs, and cardiac arrest.
Can heart block be prevented?
Pregnant mothers who are known to have an autoimmune disease may be able to receive certain treatment that may reduce the risk of heart block in their babies.
Prevention of heart block focuses mainly on managing the risk factors. A healthy lifestyle contributes to overall good health — including heart health. Exercise, eat a well-balanced diet, and don’t smoke. Understanding the risks of your medicines and reviewing them with your healthcare provider can reduce the risk of medicine-induced heart block.
Living with heart block
Follow your healthcare provider’s recommendations for taking medicine and using a pacemaker, if that applies to you. Also, always keep follow-up appointments to make sure your treatment is on track.
To improve your quality of life with a pacemaker, you may need to:
- Avoid situations in which your pacemaker may be disrupted, such as being near an electrical device or devices with strong magnetic fields.
- Carry a card that lets people know what kind of pacemaker you have.
- Tell all of your healthcare providers that you have a pacemaker.
- Get routine pacemaker checks to make sure your device is working well
- Stay active, but avoid contact sports.
- Wear a medical alert bracelet or necklace.
When should I call my healthcare provider?
Seek immediate medical attention for these symptoms:
- Extreme tiredness
- Dizziness
- Fainting or loss of consciousness
- Shortness of breath
- Chest pain
If you have sudden cardiac arrest, you will obviously not be able to seek care for yourself. It is critically important to make sure the people you see on a regular basis know what to do in an emergency. Calling 911 is the most important first step.
Key points
- Heart block occurs when the electrical signals from the top chambers of your heart don’t conduct properly to the bottom chambers of your heart.
- There are three degrees of heart block. First degree heart block may cause minimal problems, however third degree heart block can be life-threatening.
- Heart block may cause no symptoms or it may cause dizziness, fainting, the feeling of skipped heart beats, chest pain, difficulty breathing, fatigue, or even cardiac arrest
- Depending on your degree of heart block, you may not need treatment, but for some, a pacemaker is advised.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.