Revolution in American Medicine
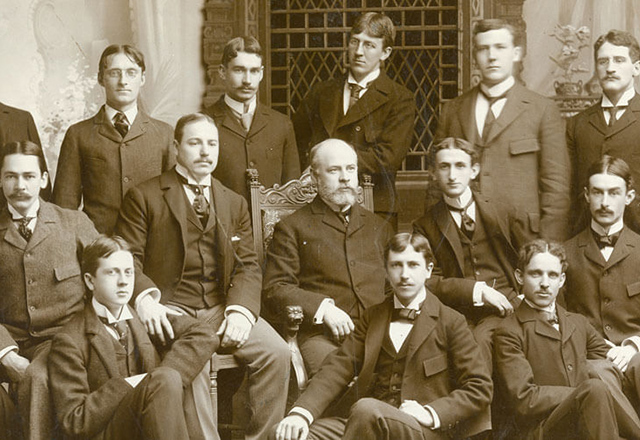 The first graduating class of the School of Medicine.
The first graduating class of the School of Medicine.The Johns Hopkins Hospital earned its reputation by radically transforming medical education and the practice of medicine and medical research. With the opening of the hospital in 1889, followed four years later by the School of Medicine, the institution revolutionized American medicine with:
- Rigid entrance requirements for medical students.
- A vastly upgraded medical school curriculum with emphasis on the scientific method.
- The incorporation of bedside teaching and laboratory research as part of the instruction.
- Integration of the school of medicine with the hospital through joint appointments.
The new model also created standardized advanced training in specialized fields of medicine with the creation of the first house staff fellowships and postgraduate internships.
The vision was an American medical institution modeled on German universities, where medical science was highly valued and laboratories were well equipped. Few facilities like this were available in the United States in the late 19th century, but slowly, with The Johns Hopkins Hospital in the vanguard, society came to understand that medicine could not advance without doctors firmly grounded in basic science and applied research methods to study of the cause and prevention of disease.
Johns Hopkins recruited four impressive young physicians, William H. Welch, William Osler, William S. Halsted and Howard Kelly — the so-called Big Four — by offering them rare and tempting research opportunities. At Johns Hopkins, basic scientists, and later clinicians, were free to do research by having a full-time salary, a departure from the tradition of employing part-time local practitioners to teach classes.
Fortunate Timing
The opening of The Johns Hopkins Hospital was delayed for 13 years after that of the university in 1876. These years gave Daniel Coit Gilman, the university's first president, time to create a novel program of postgraduate education.
The delay also gave William H. Welch, the first professor at the School of Medicine, a chance to get pathology up and running before the wards opened.
An emphasis on research was well established at The Johns Hopkins Hospital before a single patient was admitted. With Robert Koch’s discovery of the tuberculosis organism in 1881, the institution furthered awareness of the role of germs in disease, which strongly influenced the practice of medicine.
The School of Medicine opened four years after the hospital, allowing Johns Hopkins’ innovative residency system time to prove its effectiveness and provide a path for the first medical students to go to work in the wards. The gap also gave William Osler the time he needed to write his classic textbook, The Principles and Practice of Medicine.
Tougher Requirements, Better Practitioners
Before the ascendency of The Johns Hopkins Hospital, it was easy to become a doctor. Most medical students were taught in for-profit "trade schools" that often accepted high school graduates who would have had trouble getting into a liberal arts college. After two or three years of attending repetitious lectures by part-time teachers, students were free to apprentice themselves to older doctors or simply hang out a shingle, even if they had never laid a hand on a patient.
The Johns Hopkins medical school asked a lot more of its applicants: All students were required to have a college education and pass rigid entrance examinations that were heavy on basic science — chemistry, physics and biology.
The Birth of the Clinician-Scientist
 The Halsted operating team.
The Halsted operating team.At Johns Hopkins, classes were small and involved hands-on training with patients, a departure from the old lecture format. From the start, women were permitted to enroll if they met the same entrance requirements as men, breaking a longtime barrier. The educational process fostered medical research by both faculty and students and put it on par with patient care. Creating “clinician-scientists” became a Johns Hopkins hallmark.
Study was rigorous and lasted four years, including unprecedented hours of bedside learning at the side of experts, original research projects guided by respected clinicians, and extensive laboratory training.
Increasing Influence at Other Medical Schools
Then came postgraduate education in The Johns Hopkins Hospital for interns and residents, an innovation that became the model for the postgraduate clinical education of the 20th century. Those who completed Johns Hopkins' program were soon in demand across the country.
In 1910, when the Carnegie Foundation asked educator Abraham Flexner to survey the 150 medical schools then operating in the United States and Canada, Flexner found only five that he thought were adequate.
He held up Hopkins as the model: "The influence of this new foundation can hardly be overstated," Flexner wrote. “[Johns Hopkins] has finally cleared up the problem of standards and ideas, and its graduates have gone forth in small bands to found new institutions or to reconstruct old ones."
In fact, Washington, Vanderbilt, Iowa, Duke and Rochester universities patterned their medical schools directly after Johns Hopkins. Duke hired all but one of its first chairs and chiefs of service from among Johns Hopkins faculty.
To this day, Johns Hopkins has been among the top medical schools in the amount of competitive research grants awarded by the National Institutes of Health.
