Immunometabolism
The Immunometabolism Program at the Bloomberg~Kimmel Institute for Cancer Immunotherapy is investigating ways to target the metabolism of both tumor cells and immune cells to enhance immunotherapy.
Metabolic programming — getting cells the fuel and building blocks they need to grow — is essential to the function of both the tumor and the immune system. Tumors grow because the cells continue receiving the large quantities of proteins, lipids and DNA. Cancer needs so many more of these nutrients than normal cells, that it’s easy to exploit the difference. Even if you cut off the supply line to the tumor, growth can be slowed without harming normal cells.
Erika Pearce, Ph.D. and Edward Pearce, Ph.D., jointly head the Immunometabolism Program at the Bloomberg~Kimmel Institute for Cancer Immunotherapy.
Program Co-Leaders
The Bloomberg~Kimmel Institute: Dr. Jonathan Powell
Dr. Jonathan Powell, previous leader of the Metabolism Program and former Associate Director of The Bloomberg~Kimmel Institute for Cancer Immunotherapy at The Johns Hopkins Kimmel Cancer Center, explains immune therapy and how it is used to treat many types of cancers.
Combining Metabolism-Interfering Drugs with Immune Checkpoints
The BKI team is working to better understand the metabolic pathways that supply nutrients to cancer cells and immune cells, so they can develop drugs that interfere with the pathways that help nourish tumors.
It’s a similar methodology to the immune checkpoint blockade anti-PD-1. In fact, combining these nutrient-blocking therapies with a checkpoint blockade delivers a one-two punch to cancer cells: first the cancer cell is weakened by malnourishment, and then the blockade goes to work killing the weakened cells.
 Jonathan Powell, M.D., Ph.D., former leader of the Immunometabolism Program, and Barbara Slusher M.A.S., Ph.D.
Jonathan Powell, M.D., Ph.D., former leader of the Immunometabolism Program, and Barbara Slusher M.A.S., Ph.D.Immunometabolism Program
What is immunometabolism?
This emerging field is built on the idea that by understanding and targeting both the metabolism of the tumor (the bad guys) and the immune cells (the good guys) we can markedly enhance the success of immunotherapy.
What does it have to do with cancer?
Tumors need energy and building blocks to grow and multiply: proteins, lipids, DNA. By blocking their ability to receive these nutrients, they become weaker and vulnerable to cancer-killing immune cells.
What are the program goals?
Build cells that are “dressed to kill” — enhance the metabolic programming of cells to make their cancer-fighting abilities more potent
Make immune cells that are “built to last” — figure out how to prepare the immune system in advance so it’s ready to act if cancer cells appear
What have researchers at Johns Hopkins learned so far?
Cancer cells require a lot of nourishment to grow and spread. Far more than regular cells. Knowing this, we can exploit the differences by targeting the metabolic pathways that serve as a lifeline to tumors. Starve the tumor, weaken the cells, and let the immune system finish the job.
What's next?
- Collaborate with the other cancer immunotherapy scientific programs to learn more about the mechanisms that allow tumors to evade immune system attack.
- Create new ways to intervene in immune therapy treatment to increase the number of patients who can be successfully treated.
- Metabolism will play a big role, both in tumor and immune cells.
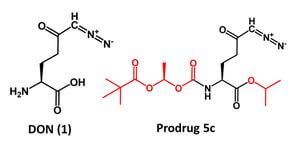
Scientists Build a Better Cancer Drug to Pass Through Blood-Brain Barrier
In efforts to develop new treatments for brain cancer, scientists from Johns Hopkins Drug Discovery and the Kimmel Cancer Center's Bloomberg~Kimmel Institute for Cancer Immunotherapy report they have altered the structure of an experimental drug that seems to enhance its ability to slip through the mostly impermeable blood-brain barrier.
Advances in Drug Development
The Immunometabolism Program is collaborating with the Bloomberg~Kimmel Institute’s Drug Development Technology Center to develop a novel drug that attacks the glutamine metabolism of the tumor, inhibiting tumor growth and making the tumor more susceptible to immune attack.
Dr. Powell is also studying a group of drugs originally developed for Parkinson’s disease that target the adenosine pathway, which acts as an on/off switch for immune cells. Preclinical study results show that the adenosine-inhibiting drug sparked an immune response against cancer cells. Now, the company that made the drug is running a multi-site clinical trial that includes the Bloomberg~Kimmel Institute.


