Immunoengineering
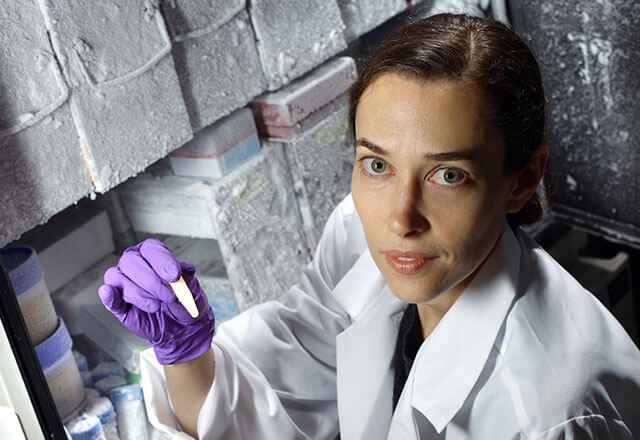 Jennifer Elisseeff, Ph.D., leads the Immunoengineering Program at the Bloomberg~Kimmel Institute for Cancer Immunotherapy.
Jennifer Elisseeff, Ph.D., leads the Immunoengineering Program at the Bloomberg~Kimmel Institute for Cancer Immunotherapy.The Immunoengineering Program at the Bloomberg~Kimmel Institute for Cancer Immunotherapy has emerged as a link between the fields of biomedical engineering and immunotherapy. Led by Jennifer Elisseeff, Ph.D., director of the Translational Tissue Engineering Center, the program’s work stems from discoveries made during her study of bioengineered tissue as a treatment for trauma injuries.
Exploring the Anti-Cancer Potential of Biomaterials
When implanted at an injury site, these biomaterials create an immune response that stimulates immune cells to treat the injury. Dr. Elisseeff’s team is conducting animal studies with melanoma cells to explore whether these same biomaterials might be used to create an anti-tumor response. After injecting biomaterials in mice that had been engrafted with melanoma skin cancer cells, the team observed a slowing of tumor growth and immune changes in lymph nodes both at the injection site and elsewhere in the body — suggesting that these biomaterials may also be able to find and kill cancer cells that have spread from the primary tumor site.
Immunoengineering researchers hope to move into human clinical trials after the safety and efficacy of the biomaterials on trauma patients is established in a separate study.
Elisseeff Lab
Principal Investigator
Jennifer Elisseeff, Ph.D.
The mission of the Elisseeff Lab is to engineer technologies to repair lost tissues. We aim to bridge academic research and technology discovery to treat patients and address clinically relevant challenges related to tissue engineering. To accomplish this goal we are developing and enabling materials, studying biomaterial structure-function relationships and investigating mechanisms of tissue development to practically rebuild tissues. The general approach of tissue engineering is to place cells on a biomaterial scaffold that is designed to provide the appropriate signals to promote tissue development and ultimately restore normal tissue function in vivo. Understanding mechanisms of cellular interactions (both cell-cell and cell-material) and tissue development on scaffolds is critical to advancement of the field, particularly in applications employing stem cells. Translation of technologies to tissue-specific sites and diseased environments is key to better design, understanding, and ultimately efficacy of tissue repair strategies. We desire to translate clinically practical strategies, in the form of biomaterials/medical devices, to guide and enhance the body's natural capacity for repair. To accomplish the interdisciplinary challenge of regenerative medicine research, we maintain a synergistic balance of basic and applied/translational research.

Immunoengineering Program
What is immunoengineering?
Using bioengineering tools — biomaterials, nanoparticles, and drugs that could be incorporated into those materials — to make the immune system attack tumors or to create more regenerative microenvironments.
What does it have to do with cancer?
It’s an emerging field, but there’s a clear connection between how a wound and a tumor each respond immunologically to biomaterials. This discovery could mean that treatments designed to heal trauma wounds could be re-engineered to fight cancer.
What are the program goals?
Use nanotechnology to deliver drugs to immune cells in a way that augments the desired anti-tumor response. Study the immune response to biomaterials and leverage that knowledge to fight cancer and regenerate tissue.
What have researchers at Johns Hopkins learned so far?
Biomedical engineers were studying soft tissue reconstruction for trauma patients and discovered that the pro-regenerative properties of the biological materials were caused by the immune response to the materials. With the growing interest in cancer immunotherapy, researchers turned their attention to cancer. Can these same biomaterials be used to redirect and modulate the immune response to cancer cells?
What's next?
- Evaluate the results of human studies on the safety and activity of biomaterials for trauma victims. If successful, transfer the technology to cancer patients.
- Study the effects of the microbiome on biomaterial immune responses.
- Explore the unique properties of synthetic biomaterials, which are frequently used for drug delivery.
In the meantime, the team is working with cancer immunology experts Drew Pardoll, M.D., Ph.D., and Jonathan Powell, M.D., Ph.D., to evaluate the potential for combining biomaterials with immune therapies.
Nanoparticles for Drug Delivery
The Immunoengineering Program is also investigating how to use nanoparticles — structures 100 times smaller than the size of a single cell — to deliver immune and other therapies directly to cancer cells. Nanoparticles may someday be instrumental in treating cancer patients with biomaterials.

Healing Cancer
Biomedical engineer Jennifer Elisseeff was working on a way to promote healing in trauma patients when a friend of a cancer patient visiting Elisseeff’s lab told her that similar approaches were reported to fight cancer.
A few years later, Elisseeff began research that promised to bridge the fields of immunology and biomedical engineering. She called the emerging field regenerative immunology. It led her to a new use for her trauma-targeted therapy.
Read the full story in a special issue of Promise & Progress.
