Mammogram 101: Q&A with a Mammographer
Did you know you don’t need a referral, prescription or order form from your doctor to get a mammogram? Women over 40 who are not experiencing symptoms can make an appointment for their annual mammogram on their own.
Annual mammograms are the best tool for early detection of breast cancer. Most cancers detected by mammography have no symptoms.
To give you a behind-the-scenes perspective of your annual mammogram, a mammographer from Johns Hopkins Medical Imaging, answers some commonly asked questions about how to prepare for your mammogram, who conducts them, who reads them and what happens after your exam.
What should I do to prepare for my mammogram?
Once you make your appointment for your annual mammogram, you don’t have to do much. Breasts can be tender the week before and during menstruation, so try to schedule your mammogram for one to two weeks after your period starts. We ask women to not wear deodorant, powder, lotion or perfume on the day of their exam as they could show up on the mammogram. For your comfort, we recommend wearing a two-piece outfit, so you are able to keep your pants or skirt on during the mammogram.
If you are breastfeeding or think you may be pregnant, please check with your doctor before scheduling your exam.
Who performs my mammogram?
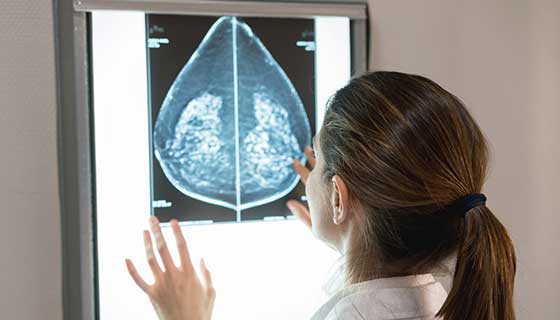
Mammograms are done by licensed, board-certified technologists called mammographers. Mammographers are specially trained to perform and review breast images of the highest quality with the least amount of radiation exposure. Johns Hopkins mammographers are subspecialized and only conduct breast exams.
We want patients to know that “as a mammographer, I am here to work with you to make this experience as comfortable as possible, to obtain a quality mammogram and ensure your breast health is taken care of.”
Who interprets my mammogram images?
You may never meet your radiologist, but the radiologist is a critical part of your health care team, working with your doctor to keep you healthy or find out why you are sick. Radiologists interpret mammogram and other screening and diagnostic images.
Radiologists are doctors who have continued their education to complete a four-year residency in radiology. A radiologist may act as a consultant to your doctor, or act as primary doctor in treating a disease.
Johns Hopkins breast imaging radiologists are subspecialty radiologists. This means they are fellowship trained, which provides additional training in all aspects of a specific body area or condition, and only read images in that area of expertise. Johns Hopkins breast imaging radiologists only read breast images and are able to focus on the unique aspects of each breast image. Studies have shown that subspecialist radiologists detect more cancers and more early-stage cancers and have lower callback rates than general radiologists.
Karen Horton, director of Johns Hopkins Medicine’s Department of Radiology and Radiological Science, explains the radiologist’s role: “I view myself as a detective trying to diagnose the patient’s problem by combining medical images with other information in the medical record to solve the mystery. Radiology is a unique medical specialty because we use imaging technology to see what is happening on the inside of the body to diagnose and treat disease. We combine high-resolution images with multiple sets of medical record data (patient history, symptoms, demographics, etc.) to determine why a patient is ill to help the referring physician chart the best plan of action to heal the patient.”
What happens after my mammogram?
There is typically no special type of care following a mammogram. However, your health care provider may give you additional instructions depending on your specific health condition.
The radiologist will send the report to your doctor and be a resource in creating an action plan if needed. If you are asked to come back for additional images, don’t be alarmed. In the United States, approximately 5 to 15 percent of women are called back for additional imaging. Additional images might be another mammogram or a different imaging method, such as ultrasound or MRI. The findings of this additional imaging are usually benign, meaning the changes are not caused by cancer.
What happens to the images?
The majority of women will have benign changes in their breasts caused by hormones or the aging process. Through yearly mammograms, these changes can be tracked and monitored. Previous images will be used as a resource to monitor any changes in the breast and flag suspicious changes.
What can I do to be proactive in my breast health if I’m not 40 yet?
Your health care provider should perform a clinical breast exam at your annual physical, and you can practice breast self-awareness by knowing what is normal for your breast and being able to identify small changes immediately. You should perform breast self-exams at least once a month at the same time frame in your menstrual cycle.
Women who are at an increased risk of breast cancer should talk with their health care providers about starting mammography screening earlier than 40, having additional tests (such as breast ultrasound or MRI), or having more frequent exams.
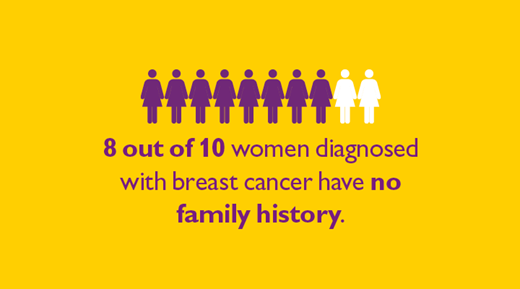
Increased risk can include:
- Family history
- Genetic tendency
- Breast density
- Past breast cancer
Eight out of 10 women who are diagnosed with breast cancer have no family history; being proactive about your breast exam is a critical step in your overall health.