Johns Hopkins Pancreas Islet Transplant Program
Our program offers a procedure for people who need pancreas removal due to conditions such as pancreatitis. We were the first in the U.S. to perform laparoscopic and robotic versions of this procedure.
About Total Pancreatectomy and Islet Autotransplantation
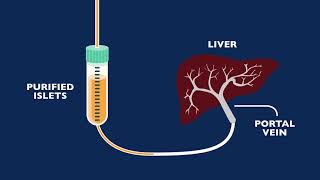
Total pancreatectomy means removal of the pancreas. Pancreas creates digestive enzymes for food digestion and insulin to control blood sugar. To compensate for the missing pancreas, insulin-producing cells in the pancreas (islets) are transplanted to the liver. The pancreas is processed in a machine that isolates the islets, which are then placed in an IV bag with a solution and infused into the liver.
Why Choose Johns Hopkins Islet Autotransplant Program?
Multidisciplinary Team
Advanced Treatments

Groundbreaking Research
Meet Our Specialists
Nurse Practitioner Staff
Christi Walsh, MSN, CRNP
Johns Hopkins Hospital
Baltimore, MD

Frequently Asked Questions
Learn more about why total pancreatectomy and islet autotransplantation may be necessary.
-
You may benefit from total pancreatectomy and islet autotransplantation if you have:
- Acute pancreatitis that keeps coming back and affects your quality of life
- Painful chronic pancreatitis that didn’t improve after other treatments
- Inherited pancreatitis that may increase your risk of pancreatic cancer
This procedure may offer best results for people with pancreatitis due to genetic mutations and not related to alcohol use or smoking. Those whose pain and opioid use has not been prolonged may also see better outcomes. On average, pain lessens in 80 percent of patients after pancreas removal, and some have no pain.
-
During your consultation appointment, you will meet separately with a gastroenterologist, a surgeon and an endocrinologist to discuss your symptoms and medical history. The doctors may also ask you to get certain tests done, such as bloodwork, to assess the function of the pancreas. Our team will then evaluate your case and determine the risks and benefits of this procedure. We will let you know if you are a candidate or if another treatment may offer better results.
-
If you are a candidate for islet autotransplant surgery, you may also be candidate for laparoscopic islet autotransplantation, which is a minimally invasive procedure. Several factors can affect your eligibility, including having extensive prior surgeries, presence of scar tissue, and body weight.
-
The islet autotransplant procedure uses your own tissue so there is no wait time.
-
As with any other surgery, there is a risk of infection, bleeding and death. Other risks include becoming diabetic and requiring lifelong use of insulin to control blood sugar levels.
-
You will be in the intensive care unit for approximately 2-4 days after the procedure. You may spend another 6-10 days in the hospital for adequate rest and healing.
After you are discharged from the hospital, you will not be able to drive or lift anything over 10 pounds for 6-8 weeks. You will be able to go up and down steps and should be able to eat a regular diet. You may have a home care nurse assist you if you require insulin.
-
You will have follow-up appointments scheduled for two and four weeks after you have been discharged, then three, six, nine, and 12 months after the surgery. Moving forward, you may have one annual follow-up visit.