With the goal of improving health outcomes for our patients and communities, we implement and optimize a strategic, innovative, and data-driven population health operating model across the continuum of care.
The Johns Hopkins Medicine Office of Population Health (OPH) is a Johns Hopkins Health System department comprised of management and patient-facing clinical teams. Together, these teams support enterprise-wide efforts to:
- Improve quality and patient outcomes by implementing timely and site-appropriate care delivery and utilization management
- Implement, strengthen and evaluate data-driven and population health models of care and manage value-based care programs
- Reduce health disparities by increasing patient access to services and advancing care integration
OPH’s principles




Evaluate Program Impact Through Data and Analytic Transformation
- Identify patient groups and actively manage and guide them through clinical interventions.
- Determine risk and return on investment.
- Evaluate population-based total cost of care use targets trended performance across the continuum of care and develop Performance Incentive Programs (PIPs).
Financial Transformation
- Leverage enterprise-wide intelligence to identify key cost drivers and evaluate use trends.
- Conduct impact analysis of the Care Transformation Organization (CTO) care management model to inform performance improvement and optimize resource allocation.
- Align our activities to perform under the total cost of care reimbursement model.

Care Model Innovation
- Accelerate population-based models of care based on their potential impact.
- Align clinical interventions and associated models of care to attributed populations.
- Leverage data liquidity to understand interrelationships between utilization/cost and quality indicators through Health Care Effectiveness Data Information Sets.

Value Streams
Program Leadership
Provide leadership and accountability for the Johns Hopkins Medicine Alliance for Patients Care Transformation Organization (CTO) and the Diabetes Prevention and Education Program (DPEP).
Value-Based Care Expertise
Data Analytics
Clinical Services
Health System Coordination
collaborations Our Population-based Interventions
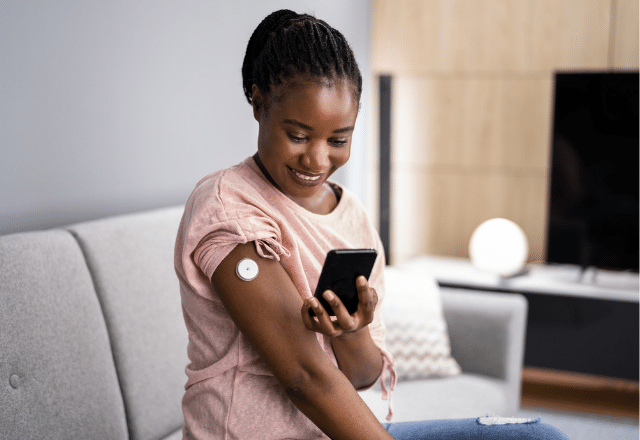
JHM Diabetes Prevention and Education Program
The Johns Hopkins Medicine Diabetes Prevention and Education Program (DPEP) is home to the CDC’s National Diabetes Prevention Program and the American Diabetes Association-recognized Diabetes Self-Management Training programs. DPEP focuses on preventing diabetes onset and using evidence-based practices to empower people with diabetes and pre-diabetes to manage their health.
Post-Acute Care Collaborative
The Office of Population Health manages the Post-Acute Care Collaborative (PACC). The PACC drives quality improvement in post-acute transitions and care throughout JHHS, and develops innovative strategies to improve transitions and reduce hospitalizations.
Cross-Functional Care Coordination
Interdisciplinary care management teams embedded at CTO-participating primary care practices collaborate to furnish an array of care coordination services, including high-risk patient management, integrated behavioral health, ambulatory pharmacy, ambulatory care management health care navigation and resource support.

