Surgical Education
How can you best assess surgical skills in the operating room?
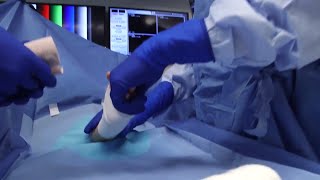
Assessing surgical skills in the operating room remains a challenge. Therefore, we created an electronic resource to help ensure that the plastic surgery training program stays compliant with changes mandated by the Next Accreditation System (NAS) Milestones and the Accreditation Council for Graduate Medical Education (ACGME). MileMarkerTM is the web-based tool we use to assess plastic surgery residents. It is made up of the Operative Entrustability Assessment (OEA), a rapid electronic assessment of resident operating room performance completed after each surgery; a data dashboard displaying graphical summaries of resident progress by case and NAS Milestone group; and an electronic Milestones tracker. All of these help us perform ongoing trainee assessments of residents’ data in the operating room. This gives immediate feedback to trainees, creates assessment transparency, lets trainees self-monitor their progress, and informs end-of-rotation reviews, program-wide assessments, and tailor training to address specific needs.
The Operative Entrustability Assessment (OEA) showed its value in a study of autologous breast reconstruction and hand surgery cases, demonstrating that higher OEA scores are associated with shorter operative times. Additionally, the OEA score was a better predictor of shorter operative time than the resident’s post-graduate year (PGY, or level of training).
Learn more about Dr. Lifchez's work on the Milemarker Assessment Tool.
#TomorrowsDiscoveries: MileMarker Improving Resident Performance – Scott Lifchez, M.D., FACS
Dr. Scott Lifchez and other faculty members have developed a one-minute assessment that is used to rate a resident’s performance after every surgery on any mobile device.
What operative performance feedback do you provide to residents?
Feedback on a resident’s operative performance is essential for surgical training. We have done multiple studies evaluating surgical resident and fellow perspectives on their needs for operative performance feedback. We have also looked at whether timeliness of attending-provided feedback has an effect on the reliability of that feedback. These studies have shown that residents and fellows find verbal, face-to-face feedback very or extremely important and prefer that feedback be given during or immediately after cases. However, surgical trainees still value feedback given within one week of the event. Our research also demonstrates the reliability of OEA evaluation scores that attending surgeons give their residents until two weeks after completion of the surgical case.
Trends in Operative Performance for Independent and Integrated Training Programs
Plastic surgery training can be completed by following either of two paths: (1) the independent pathway, which includes completing a general, orthopedic, or other surgery residency and an additional 3 years of plastic surgery training; or (2) the integrated pathway, which includes 5 or 6 years of plastic surgery training without prior completion of a surgical residency. Many plastic surgery training programs are eliminating their independent training pathways. Examining differences between independent and integrated residents may help programs determine whether to keep independent training pathways. This study aimed to differentiate between integrated (PGY4-PGY6) and independent (PGY1-PGY3) plastic surgery residents regarding their operative competency. OEA data demonstrated that independent plastic surgery residents perform at a slightly lower level than their integrated colleagues do during the first three quarters of their first year. However, they show a similar level of competency after this period. This indicates minimal drawbacks with regards to surgical skills to having both types of residents in plastic surgery training programs.
Does resident involvement affect surgical care?
Periodically, patients have concerns about having resident involvement in their surgical care. Although some studies have examined postoperative outcomes associated with resident participation in certain surgical procedures, the association between resident involvement and surgical morbidity in immediate breast reconstruction is not well documented.
We did this study to see whether resident involvement in immediate breast reconstruction would be correlated with an increase in 30-day surgical morbidity, readmission and reoperation rates, operative time, and length of stay. We found that in immediate breast reconstruction patients, resident involvement was not associated with any of those measures.. However, operative time was greater when residents were participating, although the amount of time differed according to resident training level. These findings were statistically significantly. These data support the safety of involving residents in the surgical care of immediate breast reconstruction cases, and could be used in counseling patients who might have concerns about having residents participate in their surgical care.