-
Nasir Islam Bhatti, MD

- Director Johns Hopkins Percutaneous Trach Service
- Associate Professor of Otolaryngology-Head and Neck Surgery
-
James H. Clark, MBBChBAO

- Co-Director, Johns Hopkins Dysphagia and Deglutition Clinic
- Assistant Professor of Otolaryngology-Head and Neck Surgery
-
David W. Eisele, MD
- Andelot Professor of Laryngology and Otology
- Professor of Otolaryngology-Head and Neck Surgery
-
Matthew Lewis Kashima, MD

- Director, Comprehensive/General ENT
- Assistant Professor of Otolaryngology-Head and Neck Surgery
-
Robin Yang, MD DDS
- Director of Pediatric Plastic Surgery
- Assistant Professor of Plastic and Reconstructive Surgery
-
Kevin M. Motz, MD
- Director, Division of Sleep Surgery
- Assistant Professor of Otolaryngology-Head and Neck Surgery
Wake up with the energy to take on the day
The Johns Hopkins Center for Snoring and Sleep Surgery provides comprehensive surgical and dental care for patients with obstructive sleep apnea (OSA) or snoring who have not had successful medical treatment or are interested in exploring other treatment options.
Explore On This Page:
Schedule an Appointment
Schedule by phone
Call 443-997-6467
Schedule online through MyChart
Some services may not be available for online scheduling.
Log into MyChart
| Sign up for MyChart.
Hypoglossal Nerve Stimulation for Obstructive Sleep Apnea | David’s Story
David’s obstructive sleep apnea (OSA) left him unable to sleep well at night for the past 30 years. Learn how sleep surgeon Kevin Motz helped David finally get a good night's rest.
Our Services
Our multidisciplinary team of surgical providers works with you to develop an individualized treatment plan to address your sleep apnea or snoring problems. This may include a comprehensive history and physical examination including an airway evaluation and surgeries. The type of surgery recommended to you may include:
Nasal Surgery
- Septoplasty
- Nasal turbinate reduction
- Nasal valve reconstruction
Palatal Surgery
- Uvulopalatopharyngoplasty (UPPP)
- Tonsillectomy
- Palate radiofrequency
- Palatal implantation
- Expansion Pharyngoplasty
Base of Tongue Surgery
- Lingual tonsillectomy
- Partial midline glossectomy
- Radiofrequency to the base of tongue
- Genioglossal advancement
- Hyoid myotomy and suspension
- Tongue suspension suture
Other Surgical Procedures
- Maxillomandibular advancement
- Tracheostomy
- Limited uvulopalatopharygoplasty
- Custom oral appliances
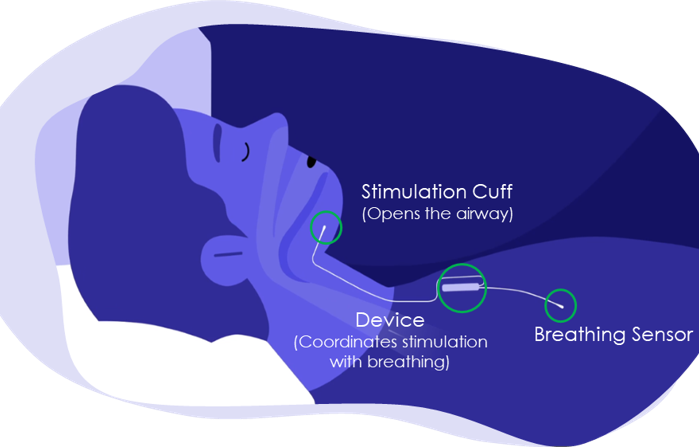
New Treatment: Hypoglossal Nerve Stimulator
Johns Hopkins Otolaryngology–Head and Neck Surgery’s specialists are available to provide the only FDA-approved hypoglossal nerve stimulator (Inspire®) as a possible treatment for patients with obstructive sleep apnea.
-
- It is a device that delivers upper airway stimulation
synchronized to your breathing to relieve obstruction
during sleep. - It is inserted during an outpatient procedure.
- You control the device using a hand-held sleep remote.
- It is a device that delivers upper airway stimulation
-
Hypoglossal nerve simulation surgery offers an innovative neuro-stimulatory approach to relieving upper airway obstruction in patients with obstructive sleep apnea. This device can relieve sleep apnea without need to surgically remove obstructive tissue in or around your airway. Additionally, hypoglossal nerve stimulation can be used to safely monitor users with DOT or commercial drivers licenses.
-
Medicare and most insurance plans cover this FDA-approved treatment.
-
- Have moderate to severe obstructive sleep apnea (AHI 15-65 with <25% central and mixed apnea).
- Are intolerant of, or unable to get consistent benefit from, continuous positive airway pressure (CPAP).
- Are not significantly obese (BMI < 35)
- Are at least 18 years of age
- Qualifying drug-induced sleep endoscopy examination