Novel Immunotherapy/Targeted Therapy Combination Extended Survival in Some Patients With Lethal Biliary Tract Cancers
05/01/2020
A randomized, multicenter study of a combination of immunotherapy with a targeted therapy improved cancer control for some patients with a rare and lethal type of gastrointestinal cancer known as biliary tract cancers (BTCs). This is an aggressive cancer for which the standard treatment for the majority of patients has not changed significantly in more than a decade.
The study was led by Nilofer Azad, M.D., associate professor of oncology, and Mark Yarchoan, M.D., assistant professor of oncology at the Johns Hopkins Kimmel Cancer in collaboration with the National Cancer Institute and 23 cancer centers throughout the U.S. The research tested a new immunotherapy treatment combination in BTC, a typically highly immune resistant cancer, explains Yarchoan. He will present the findings “virtually” on April 28 at the annual meeting of the American Association for Cancer Research.
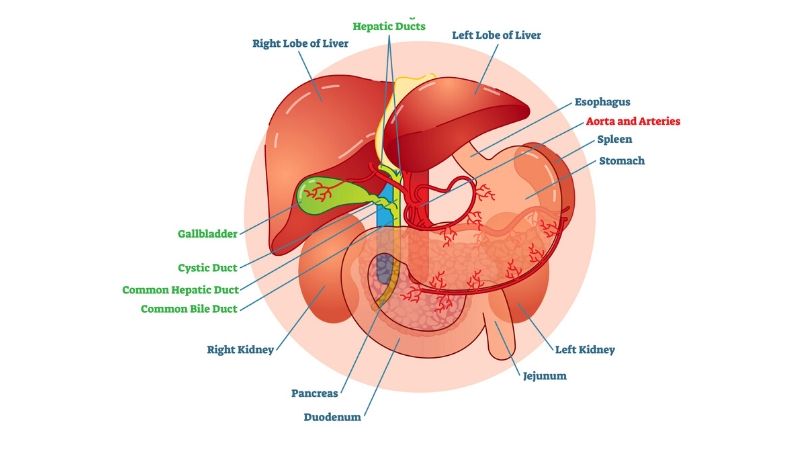
The study included 86 patients, with advanced BTC, a cancer that occurs in the ducts that drain bile from the liver. Participants were age 44 to 86, 62% (48) were female, and could have received one or two prior treatments for BTC. Patients were randomized to receive the anti-PD1 immunotherapy atezolizumab alone (single treatment arm) or atezolizumab in combination with the MEK inhibitor cobimetinib (combination treatment arm). Among the patients who enrolled on the study, 77 completed at least one dose of therapy (39 on the single treatment arm and 38 patients on the combination treatment arm). Progression-free survival in the combination therapy group was nearly double (111 days) the single treatment arm (57 days). This difference in progression free survival met the study primary endpoint and was statistically significant.
Cobimetinib blocks MEK (mitogen-activated extracellular signal-regulated kinase) which is part of a signaling pathway that is known to be overactive in BTCs. Although drugs that block MEK don’t have very much activity when used alone in BTC, they can modify the tumor environment making it more favorable for treatment with immunotherapy. Prior research found that a two-drug combination of cobimetinib and anti-PDL1 immunotherapy—drugs that remove restraints on the immune system’s response to cancer—may work together synergistically.
“We wanted to see if combining the two drugs resulted in improved anticancer activity in BTC,” says Yarchoan. To find out if the combination was effective, Yarchoan and collaborators opted to compare the benefit of immunotherapy alone to the combined therapy in a randomized study.
Side effects of the combination were manageable and included nausea, vomiting, rash, and low blood and platelet counts. There were no treatment-related deaths, but 12 patients (4 receiving atezolizumab alone and 8 receiving the combination) stopped treatment due to various side effects.
The disease control rate, or the ability to keep the cancer from growing and progressing, was 14/31 patients who’s treatment could be measured (45.2%) in the combination treatment arm, and 11/34 patients (32.4%) in the single treatment arm. Two patients, both on the combination treatment arm, remained in the study more than 15 months from study enrollment. “The low response rates in both treatment groups highlights the challenge of immunotherapy in BTC,” says Yarchoan. “However, the combination of atezolizumab with cobimetinib met its primary outcome and significantly prolonged progression free survival as compared to atezolizumab. This combination warrants further clinical investigation.”
BTC represents about 3% of all gastrointestinal cancers. The standard therapy for patients who have advanced disease is a combination of the chemotherapy drugs gemcitabine and cisplatin, but the survival of patients receiving standard treatment is less than one year. Yarchoan says that some patients with BTC may have particular mutations for which a precision medicine approach with drugs that specifically target these mutations can be beneficial. For example, a small number of patients with BTC have mismatch repair deficiency (MMR-d) in their tumor, and researchers at the Johns Hopkins Kimmel Cancer previously discovered that tumors with MMR-d can be effectively treated with anti-PD1 immunotherapy with pembrolizumab. Mismatch repair deficiency is characterized by many mutations in genes that repair copying mistakes in DNA. The larger number of mutations has been shown to attract immune cells to cancers and is a biomarker for response to anti-PD1 immunotherapy. However, the majority of patients with BTC do not have any “actionable” mutations in their tumor, and for these patients the treatment of BTC has not changed significantly since 2010, Yarchoan says.
The study was supported by the National Cancer Institute’s Cancer Therapy Evaluation Program and Experimental Clinical Trials Network, R01-CA228414-01 and UM1CA186691, and F. Hoffmann-LaRoche, Ltd.
