Earlier, More Frequent Removal of Some Pancreatic Cysts May Decrease Cancer Risk for Some Patients
05/14/2019
By analyzing medical records of 901 adults who had surgery for a certain type of precancerous pancreatic cyst, researchers at Johns Hopkins Medicine and The Karolinska Institute in Sweden have updated parameters for an anatomical “marker” that can tell more precisely if these cysts are likely to develop into lethal pancreatic cancers.
The findings, they say, are not yet proof of the concept, but do strongly suggest that removing so-called intraductal papillary mucinous neoplasms as soon as the main pancreatic duct is enlarged beyond 5 millimeters in diameter has the potential to prevent these precancers before they become malignant.
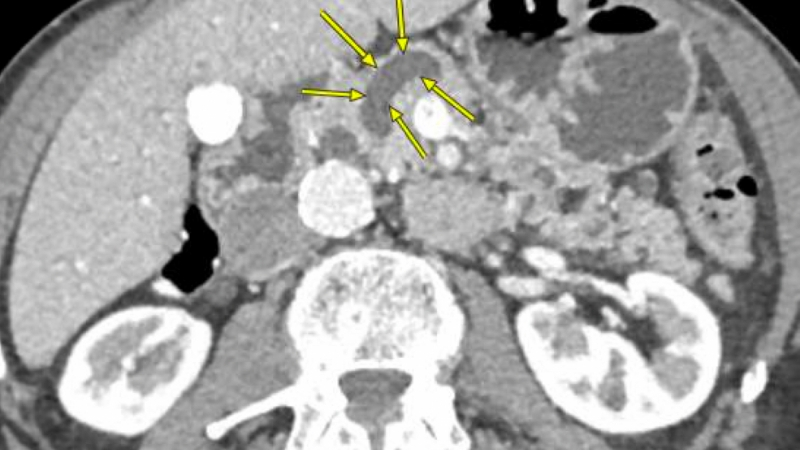
The pancreas is shaped vaguely like a revolver, with a duct --normally about 3 millimeters in diameter -- that runs all the way down the barrel of the gun and carries digestive enzymes. When inflamed or populated by cysts or other growths, the duct enlarges.
The vast majority of pancreatic cysts, including intraductal papillary mucinous neoplasms, are benign and cause no symptoms, the researchers note. In fact, most are diagnosed “incidentally” during MRIs or CT scans for non-pancreas-related conditions. But some can cause significant inflammation and damage to the duct that runs the length of the pancreas — a process that dilates, or enlarges, the duct — and are more likely precancerous or even cancerous.
Pancreatic cancer is the third leading cause of cancer deaths, affecting more than 55,000 Americans each year. The disease is difficult to diagnose and treat, and five-year survival rates after diagnosis are around 9%, according to the U.S. National Cancer Institute. As a result, efforts to identify early markers of the disease -- biological or structural -- are a priority for pancreatic disease specialists.
Guidelines set in 2012 by the International Cancer of the Pancreas Screening Consortium call for surgical removal of these cysts when there are one or more and when dilation of the duct is at or greater than 10 millimeters. But the new Johns Hopkins study findings are in support of the more recent European guidelines published in 2018, which encourage surgical removal when dilation is in a range much smaller than that.
Specifically, the researchers report in the Annals of Surgery published online this past winter, their analysis offers indirect evidence that for people who can safely undergo surgery, the best option for preventing cancer is to remove cysts when the duct is anywhere over 5 millimeters because many of those removed cysts had precancerous cells or cancer tissue.
“If we continue using the more conservative cutoff point of 10 millimeters dilation for deciding when to remove these cysts, this study suggests we will miss a lot of people who will go on to develop cancer,” says Ross Beckman, M.D., a resident and postdoctoral fellow in the Department of Surgery at the Johns Hopkins University School of Medicine and one of the lead authors on the paper. “Changing to more aggressive guidelines will lead to more surgeries, but would likely save more lives.”
For their study, the researchers collected data from the medical records of 901 patients who underwent some form of pancreas-related surgery at The Johns Hopkins Hospital between 2004 and 2017 and the Karolinska University Hospital in Sweden from 2008 to 2017. Both hospitals have the highest volume of such operations for the U.S. and Europe, respectively.
Overall, the patients’ average age was 69 years, and 52% were women.
Of the types of pancreatic surgery underwent by the participants, some 58% had Whipple procedures, which remove the head of the pancreas and parts of the small intestine and stomach, along with the gallbladder and bile duct. Another 29% had the end of the pancreas removed; 11% had complete pancreas removal; and 2% had other types of pancreas surgeries.
Each hospital used a specialized pancreatic pathologist who analyzed the cysts removed from surgery and reported the findings in the medical charts. Based on reviews of the medical charts, about 60% of the patients had noncancerous cysts, 23% had precancerous cysts and 17% had cancerous cysts.
Then, the researchers gathered information on the widths of each pancreatic duct in the 901 patients using CT scans and MRIs taken for any reason within 30 days prior to the patients’ surgeries.
The researchers found that the 286 people with pancreatic ducts dilated from 5–9.9 millimeters were 1.7 times more likely to develop precancerous cells and 3.4 times more likely to develop pancreatic cancer than people with less than 5 millimeter dilation.
Among the 150 patients with 10 millimeter or wider pancreatic ducts, the records showed they were 7.5 times more likely to develop precancerous cells and 14 times more likely to develop pancreatic cancer than the people with dilations of less than 5 millimeters.
The researchers caution that their study was designed to show associations between dilation levels and the likelihood of having or developing precancer or cancer. Their findings, they emphasize, don’t prove that removing pancreatic cysts before they dilate ducts beyond 5 millimeters will in fact prevent cancer.
But they said the findings give supporting evidence that it may be time to update the guidelines to call for surgery when dilation is in a range of 5–7 millimeters.
The researchers can’t really say for sure how many people will be saved from cancer to any certain degree as their study wasn’t designed to determine this.
“By 2025, experts predict that pancreatic cancer will be the second leading cause of cancer death in the U.S.,” says Beckman. “Since pancreatic cancer is so aggressive, survival rates remain low despite improvements in medical and surgical treatment. But one place where we may really be able to make significant improvements is in early detection and prevention — that is, removing these precancerous growths before they progress to cancer.”
If someone has a pancreatic duct dilated less than 5 millimeters, the researchers say the risk of cancer is relatively low and the risks of surgery likely outweigh the risk of cancer. In these situations, they would recommend watchful waiting with yearly surveillance with an MRI or CT scan.
Others involved in the study were Marco Del Chiaro, Zeeshan Ateeb and Urban Arnelo of CLINITEC; Nicola Orsini of Karolinska Institutet; Neda Rezaee, Lindsey Manos, Richard Burkhart, Matthew Weiss, and Jun Yu and of Johns Hopkins, including Ding Ding, Georgios Margonis, Martin Makary, Jin He, John L. Cameron and Christopher Wolfgang of the Sidney Kimmel Comprehensive Cancer Center; Roberto Valente of Sapienza University of Rome; Chunhui Yuan of Peking University Third Hospital and Lingdi Yin of the First Affiliated Hospital of Nanjing Medical University.
The research was supported by the National Cancer Institute (5T32CA126607-09), Cancerfonden Sweden (CAN 2014/634, CAN 2014/621) and ALF medel Stockholm (20150113).
The researchers don’t have any conflicts to report.
On the Web:
- Turning the Immune System on Pancreatic Cancer
- Pancreatic Cyst Clinic Gathers World-Class Experts
- Fighting Pancreatic Cancer as a Team
- Pancreatic Cancer Precision Medicine Center of Excellence gets the right treatments to the right patients at the right time
