A Cut Above — Two Devices Are Teamed to Simplify, Quicken and Improve Ear Reconstruction
09/15/2022
According to the National Birth Defects Prevention Network, one in every 8,000 to 10,000 births in the United States result in one of two congenital malformations of the ear: microtia (the child is born with only a cartilage stump for an ear) or anotia (the complete lack of an ear). Because there is no properly shaped ear canal or ear drum to capture and relay sound waves, a child with microtia or anotia usually has partial deafness as well.
Now, thanks to two novel tools developed by a Johns Hopkins Medicine resident and a former resident, the traditionally difficult surgery to create a replacement ear from a patient’s rib cartilage may soon be done faster, more simply and accurately, without wasting valuable tissue, and with the ability to “custom fit” the new organ for each patient.
“Although ear reconstruction surgery for repairing microtia and anotia in both pediatric and adult cases has been practiced for a number of years, it still is a demanding procedure for both the patient and the surgeon,” says Angelo Leto Barone, M.D., a former resident in plastic and reconstructive surgery at the Johns Hopkins University School of Medicine and now a craniofacial and pediatric plastic surgeon at Nemours Children’s Health in Orlando, Florida. “What makes it really difficult is that to construct a suitable ear requires a bit of artistic skill.”
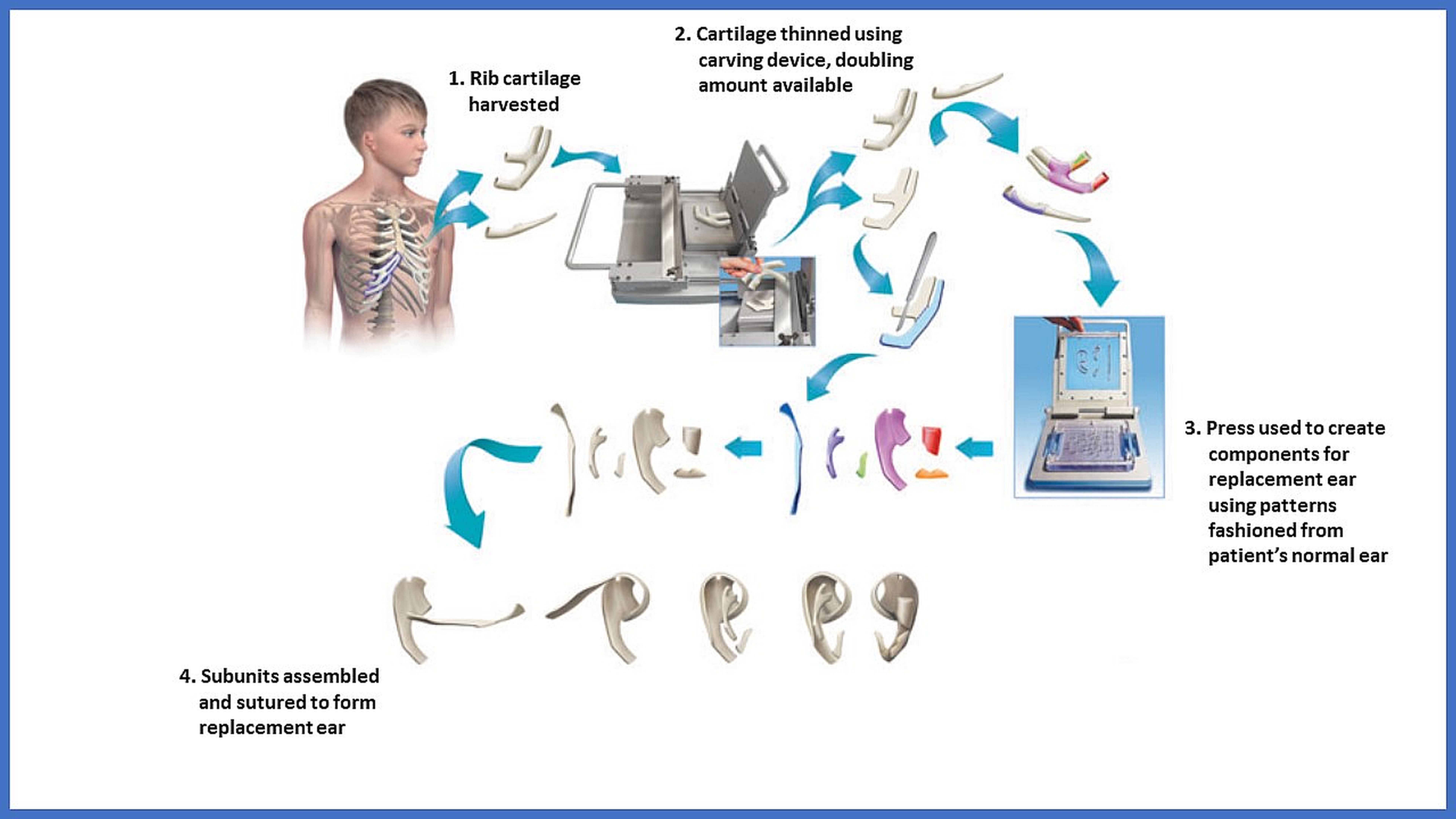
To perform an ear reconstruction without needing such innate talent, Leto Barone and his colleague, Johns Hopkins interventional and diagnostic radiology surgery resident Anirudh Arun, M.D., invented two assistive devices using 3D manufacturing. The first is a simple to use carving tool that precisely slices rib cartilage removed from the patient to any desired thickness and minimizes tissue waste. The second is a “cookie-cutter-like” press using steel blades — shaped in patterns fashioned from a patient’s normal ear — to yield the pieces of cartilage that are brought together during surgery to form the new organ.
“The cartilage-slicing device basically doubles the amount of cartilage tissue available for surgery, meaning that less has to be harvested to safely produce the entire ear,” says Arun. “We only need two and a half ribs instead of the traditional four from prior techniques — less waste and less discomfort for the patient.”
Placed into the second cutter, the cartilage slices are precisely trimmed into the components of the new ear in minutes rather than the hours needed to do it manually with a scalpel.
“Not only is the process quicker, but the template eliminates the cartilage damage that often accompanies the sculpting done in previous reconstruction methods,” says Leto Barone. “This makes our system highly reproducible, user friendly, time efficient and cost effective. Best of all, it consistently yields a natural-looking ear that helps children avoid being teased or bullied, and enables adults to do things others take for granted, like wearing glasses.”
Leto Barone and Arun recently put their assistive devices to the test in the first in-human trial of the procedure — a surgery on a teenage patient. The successful outcome is described in a research letter published in the journal Facial Plastic Surgery & Aesthetic Medicine.
“Our system did exactly what it was designed to do,” says Arun. “Compared to traditional microtia and anotia reconstruction surgery, we used less cartilage, followed a standardized procedure for constructing the ear framework and decreased the operating time required for that construction.”
Leto Barone and Arun are exploring other uses for their assistive devices by adapting them to build structures as replacements for nose cartilage, eyelids and other facial features that were malformed or missing at birth or damaged by cancer resection, burns and other disfiguring events.
A patent has been approved for Leto Barone and Arun’s two-device system.
Other authors from Johns Hopkins Medicine of the research letter are Neha Datta, Thomas Harris, Richard Redett and Jordan Steinberg. Also contributing as an author is Georges Samaha at the University of Miami Miller School of Medicine.
The project has been funded by a grant from the Limitless Tomorrow Foundation. Leto Barone, Arun and Samaha are the owners of ReconstratA, the company the owns the intellectual property rights for the microtia repair devices. Leto Barone also is the founder and president of Reconstruct Together.
