Johns Hopkins Medicine Team Creates Model to Help Show Path Toward Ending HIV Nationwide
09/23/2021
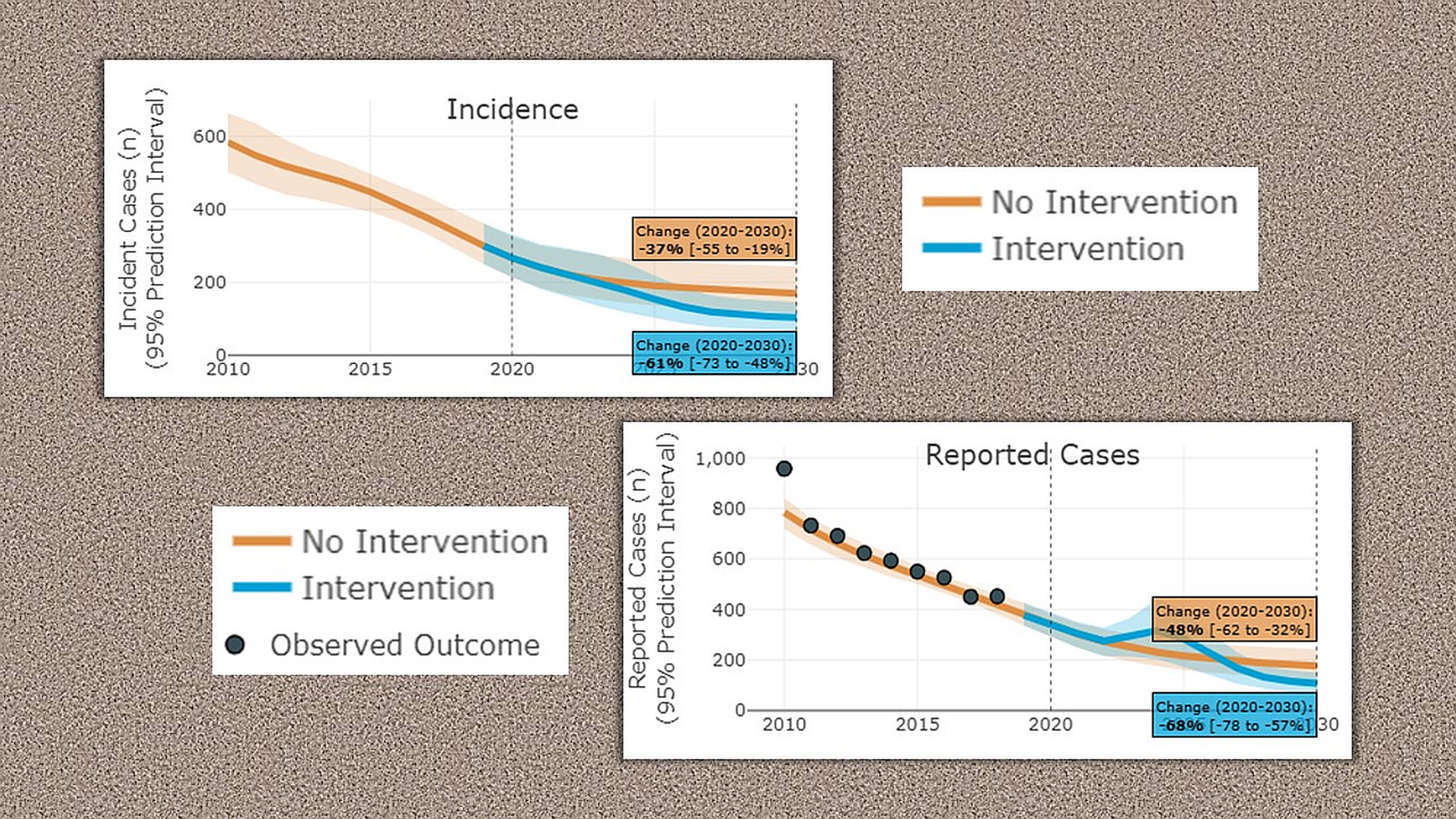
A new Johns Hopkins Medicine mathematical model to predict how the human immunodeficiency virus (HIV) spreads in urban areas will play a major role in a federal initiative aiming to reduce the incidence of HIV infections in the United States by 90% between 2020 and 2030. As part of the Ending the HIV Epidemic in the U.S. (EHE) program, the model will be used to forecast HIV incidence in 32 U.S. cities when implementing specific interventions to reduce transmission of the virus.
In a study published Sept. 21, 2021, in the Annals of Internal Medicine, Anthony Todd Fojo, M.D., M.H.S., and colleagues describe their model, an algorithm that splits each city’s population into categories of race, age, sex and HIV risk factors, and estimates the number of HIV infections associated with each one.
“We calculated the number of HIV infections per subgroup and then predicted what would likely happen if cities adopt particular interventions,” Fojo says.
Fojo says potential citywide actions could include increasing viral suppression (reducing HIV virus counts to an undetectable level) among people with HIV, more frequent testing to diagnose HIV, and encouraging the use of pre-exposure prophylaxis (PrEP) — prescription drugs that prevent HIV infection.
“For some cities, it may make more sense to focus on getting people’s HIV controlled. For others, it may be more important to encourage preventive medications,” Fojo says. “To achieve a 90% reduction over the next 10 years, the model predicts it will likely take a combination of both, along with increased testing.”
The model described in the new study shows that if current trends continue, HIV incidence overall in the 32 cities might fall by 19% by 2030. With a modest increase in testing, preventive medications and better virus suppression across the population, those cities could improve that result to a reduction of between 34% and 67%.
Predictions of drops in HIV incidence also can be estimated for interventions in specific populations.
For example, the model predicts that, if 25% of young Black and Hispanic men who have sex with men used PrEP and were tested twice a year to more rapidly identify HIV, and 90% of those already with HIV could achieve viral suppression, cities could achieve a 13% to 68% reduction in HIV incidence across the whole population.
When interventions include people who inject drugs and all men who have sex with men, the incidence of HIV could be reduced from 48% to 90%. Thirteen of the 32 cities could achieve more than a 90% reduction in incidence with large-scale interventions that include heterosexuals.
Fojo and his colleagues also have developed a web tool to help cities develop individualized plans. He says he hopes public health officials will use this resource to make cost-effective intervention decisions for their communities.
Fojo is available for interviews.
