Research Story Tip: Adult-Proven ‘Smart’ Diagnostic Tool for Diabetic Retinopathy Also Works for Kids
02/02/2021
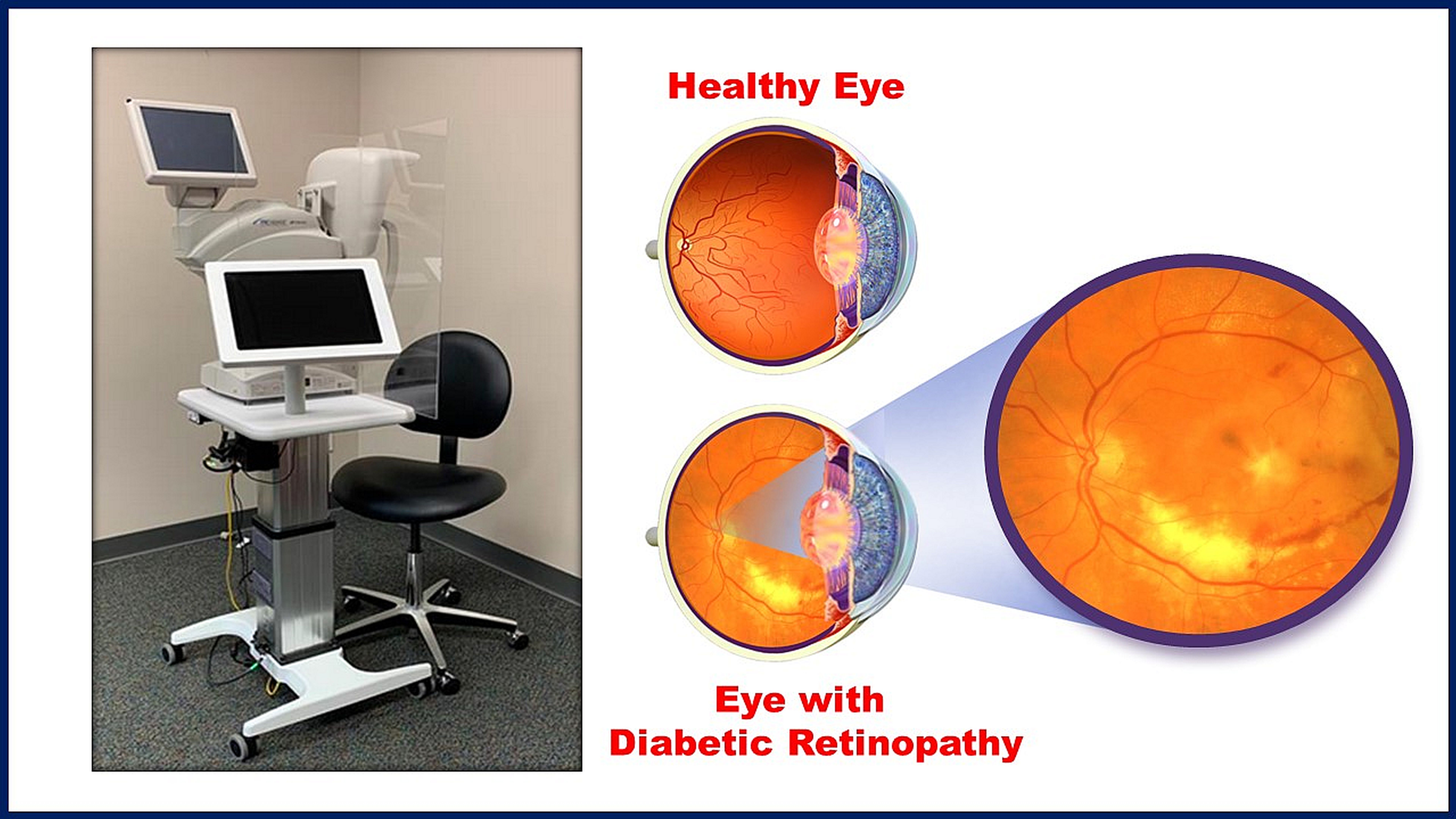
Diabetic retinopathy — a disorder characterized by damage to the small blood vessels lining the retina (light-focusing area) of the eye and a leading cause of vision loss worldwide — has been on the rise in recent years as the number of children and adolescents diagnosed with either type 1 or type 2 diabetes increases. Although the American Diabetes Association (ADA) advises regular screening for pediatric diabetic retinopathy, it’s estimated that fewer than half of all youth with diabetes follow the recommendation. Without early detection and treatment, these patients put themselves at risk for serious vision problems or blindness as they get older.
In a recent study reported online Jan. 21, 2021, in Diabetes Care, researchers in pediatric endocrinology and ophthalmology at Johns Hopkins Medicine and three other U.S. medical institutions demonstrated that autonomous artificial intelligence (AI) can be used to detect pediatric diabetic retinopathy with high sensitivity, specificity and diagnosability (accuracy of detection) — and without the need for human interpretation. The technique had already been approved for adults with diabetes by the U.S. Food and Drug Administration and is part of the ADA’s retinopathy screening guidelines for patients age 21 or older.
Because the AI screening does not require eye dilation, it takes less time to perform and is easier for pediatric patients to undergo. Therefore, the adherence of the patients in this study to getting regular retinopathy screenings, as defined by the ADA, more than doubled.
“Use of autonomous AI in adults has shown extremely high levels of sensitivity, specificity and accuracy in diagnosing referable [more than mild] diabetic retinopathy, when the disease is most treatable,” says Risa Wolf, M.D., study lead author, Johns Hopkins Children’s Center pediatric endocrinologist and assistant professor of pediatrics at the Johns Hopkins University School of Medicine. “So, with the rising incidence of pediatric diabetes — especially type 2, which is associated with an earlier onset of retinopathy — we felt it was important to see if AI could make an improvement in adherence to screening guidelines and early diagnosis for younger patients.”
A total of 310 pediatric patients with diabetes were recruited over a 12-month period for the study. The participants had a mean age of 12, were 47% male and represented a broad range of ethnicities (57% white, 32% Black, 4% Hispanic, and 7% Asian or other). Patients predominantly had type 1 diabetes (82%) and a mean age of 9 at first diagnosis of diabetes, whether type 1 or type 2.
One hundred fifty-two participants (49%) reported having a diabetic eye exam with dilation before joining the study, but only 17 (11.3%) had a record of the screening test in their case files. However, using a special statistical calculation, the researchers were able to measure the improvement in screening adherence for these patients and then estimate it for the entire group.
In the study, digital fundus photography — which does not require dilation, takes only a few minutes and produces high-quality images for detection of retinopathy by trained observers — was used in conjunction with a fully autonomous AI system built into the camera. This eliminated the need for human evaluation to get a diagnosis.
For verification of the diagnoses made by the AI system, the same color photographs were reviewed independently by two retina specialists who were not told of the AI interpretations.
Of the 310 participants, AI gave an accurate interpretation for retinopathy or no retinopathy in 302 (97.5%) cases. The eight image sets not interpreted were due to the participant’s inability to keep his or her eyes open during the photographic flash or to focus as needed.
Overall, sensitivity (85.7%), specificity (79.3%) and diagnosability (97%) of the AI interpretations in children were high, based on the reference standards for these characteristics defined by retina specialists. This high level was seen regardless of race, ethnicity, age and sex.
After implementing the AI screening system, the adherence rate improved from 49% to 95%, an increase of 111%.
“Our results show that autonomous AI — proven as a safe and effective means of diagnosing diabetic retinopathy in adults — also deserves a role in screening for this disease in younger patients,” says retina specialist Roomasa Channa, M.D., senior study author and assistant professor of ophthalmology and visual sciences at the University of Wisconsin School of Medicine and Public Health.
Wolf is available for interviews.
