Haniee Chung, M.D., has some advice for people who have been putting off colonoscopies due to COVID-19 concerns.
Don’t.
The American Cancer Society and the American Society of Colon and Rectal Surgeons now recommend that most people start getting screenings at age 45, says Chung, colorectal surgeon at the Johns Hopkins Kimmel Cancer Center at Sibley Memorial Hospital and vice director of global surgery at the Johns Hopkins University School of Medicine.
And they’re particularly important for young people, a population that’s seeing an increase in cases of colon and rectal cancer.
“Younger patients [under age 50] often don’t have symptoms, or if they do, they may dismiss them as hemorrhoids or constipation, which is why it’s important to screen patients who are having even just mild symptoms,” she says.
About 1 in 22 men and 1 in 24 women will be diagnosed with colorectal cancer in their lifetime.
Q: Why is it important that patients keep up with routine screenings such as colonoscopies during the COVID-19 pandemic?
Colonoscopy is the only way we can diagnose and treat early-stage pathology such as polyps or even early-stage colon or rectal cancer.
People should begin colonoscopies at age 45 if they do not have a family history of colorectal cancer and do not suffer from inflammatory bowel disease or have other genetic risk factors. Doctors may recommend colonoscopies at an earlier age if a patient has risk factors.
Q: What can happen if a patient puts off a colonoscopy for too long?
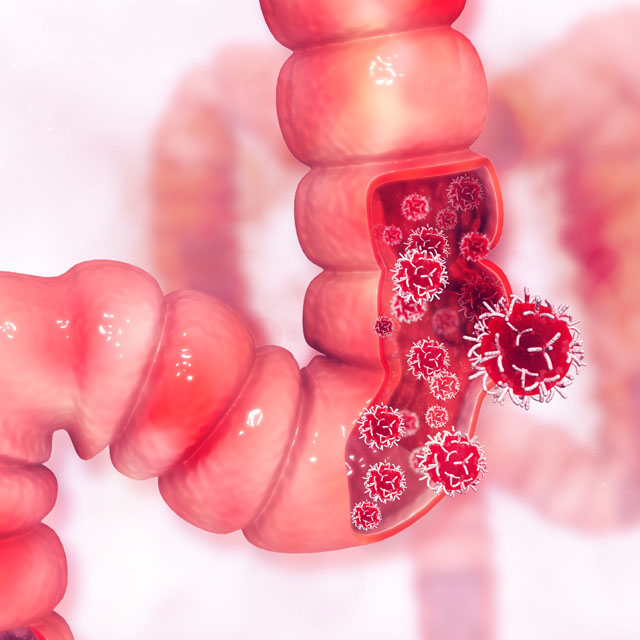
Most rectal and colon cancers develop from polyps, which can be asymptomatic at first.
If we don’t catch these early and remove polyps and small cancers, patients may need more aggressive treatment such as surgery, chemotherapy and radiation. If a cancer goes untreated for too long, it can be difficult to treat even with those options.
Q: Patients may have concerns about getting a colonoscopy during the COVID-19 pandemic. Is it safe?
Yes, we are taking all the necessary precautions and more. We’re testing all patients who come to the hospital for procedures, and we are not treating anyone who tests positive for COVID-19 until they test negative. Clinicians are outfitted with personal protective equipment.
Q: What does colonoscopy preparation involve?
It requires drinking a very strong laxative the day before, which causes the colon and bowels to empty completely. Patients can only drink clear liquid during the preparation period as well — no solid food. The preparation is probably the worst part of the colonoscopy. I recommend drinking water and electrolyte replacement drinks to avoid getting dehydrated.
Q: What happens during a colonoscopy?
The procedure itself takes about 20–40 minutes, and patients are usually under anesthesia. After doing a digital rectal exam and checking the anal skin, we use a small flexible camera to look at the large intestine, which includes the rectum and the colon. As we move the camera back out, we look for polyps and remove them, and take pictures of various parts of the digestive tract. If we remove anything like a polyp that needs to be biopsied, it usually takes a few days to get pathology results.
Q: What happens after the colonoscopy?
If we don’t find anything in the colonoscopy and the patient doesn’t have any major risk factors, then we recommend a colonoscopy every 10 years.
If we find polyps and they are benign, the recommendation could be three to five years later for the next colonoscopy. If the polyps are cancerous, the recommendation for the next colonoscopy could be as soon as six months to a year.
If we find cancer, we get additional testing — imaging and bloodwork — to determine the stage of the cancer and assess treatment options.
Q: Because they receive anesthesia, patients can’t drive after the procedure. With visitor restrictions during COVID-19, how do patients connect with their transportation home?
When the patient checks in, we will ask for the name and phone number of the person driving the patient home, and will call them when the patient is ready to be picked up. If we know how far away the driver will be, we can gauge when to call. The person giving the patient a ride will have a number to call when they arrive, and our staff will take the patient to their ride.