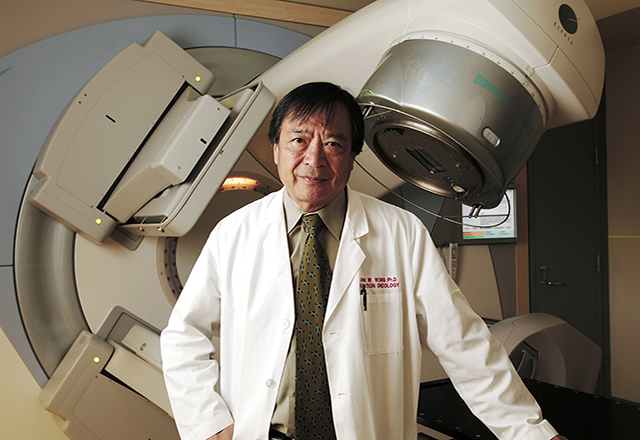
Affable and brilliant, John Wong’s energy and his excitement for the field are infectious. He moves between meetings with young up-and-coming physicists in his office to the stairwell as he scurries to the treatment areas to see his inventions in practice and interacts with clinicians who can describe existing shortfalls. Along the path, he stops to talk to faculty members, nurses, technicians, residents and fellows. He is always thinking about how he can make radiation therapy better. More impressively, he has turned these ideas into revolutionary advances in the field of radiation oncology and molecular radiation sciences.
"It's great to be paid to sit and think," he jokes.
He rarely believes a new technology is adequate “out of the box,” and proton therapy was no exception. His inventions make existing technologies better, safer and more precise. He epitomizes the intangible component so essential to proton therapy, or any radiation therapy, for that matter. It is the expertise, experience and in-depth knowledge that allow him to optimize a new technology to work better for the radiation oncologists, physicists, nurses and technicians who use it and—his main goal—to advance the care of patients.

Most places acquire proton therapy by contracting someone else to build it for them. Wong and his Kimmel Cancer Center colleagues took a different approach, partnering with manufacturer Hitachi, to design and build a one-of-a-kind proton therapy system that exceeds every other proton center in its scope, size and capability.
“We have always been innovators in the Kimmel Cancer Center. There are few places like us, but this is how leading institutions like Johns Hopkins should be driving the development of technology. When we see a clinical problem, we solve it ourselves,” says Wong. “I look for logical ways to make equipment work better, which allows researchers to dig deeper and move faster so they can get improved treatments to patients.”
Most of Wong’s inventions over more than three decades are centered on imaging that makes sure the potent radiation beam hits its intended cancer target.
John Wong's Inventions
The protection of normal tissue and organs is at the center of most everything our experts do in treating patients with radiation therapy. There is no question that radiation kills cancer cells. Researchers have understood that since 1896. At issue is how it can be used to kill cancer without harming normal cells to prevent toxic side effects at the time of treatment, particularly for pediatric and young adult patients, down the road when excess doses of radiation can result in long-term side effects or cause second cancers to develop.
The ability to direct the beam to a tumor, and only the tumor, is the advantage of proton therapy over the more scattered photon beam. However, the beam—no matter how precise—is only as good as its guidance system. Simply, put, it will hit what it’s directed to hit, which is why for most of his career, Wong has focused on the development of better imaging technologies that show where the beam is going.
The Johns Hopkins Proton Therapy Center has magnetic resonance, or MR, and CT imaging, as well as a new type of CT scan called dual energy CT that provides detailed information on the specific makeup of the tumor. This advanced and unmatched imaging makes our proton therapy the most precise of any available today.
His latest invention, the CT couch, brings new technology to photon and proton therapy by putting the image guidance directly on the therapy machines. Typically in radiation therapy, patients must move between a simulator and the treatment room. The simulator is a dress rehearsal of sorts that uses CT imaging so that the physicists and the treatment team can visualize where tumors are located in relation to the rest of the body, particularly vital organs. Complex calculations are made based on these imaging data, and the treatment plan is set in place. Until now, treatment planning and treatment delivery could not be done in the same room and usually not on the same day.
Just as the trajectory of the beam is only as good as the guidance system, the image guidance is only as good as the quality of the images it receives. Imaging resolution has been a challenge that often leads to a larger field of radiation treatment to ensure that cancer cells aren’t missed.
“Imaging is critical to the process. The better you can see the target, the more precisely you can treat with radiation,” says Wong. “If I don’t know where the tumor is, it doesn’t matter how great the equipment is.” He says proton therapy has been delivered for many years without absolutely knowing for sure where the beam is hitting.
The CT couch addresses this problem, introducing—for the first time—practical in room CT imaging. Some refer to as onboard imaging, but Wong prefers CT couch because of an essential component—the couch is part of the therapy machine, but it is not on the therapy machine so it doesn’t disturb or interfere with any of the treatment machinery. The image quality is comparable to diagnostic quality CT and far superior to cone beam computed tomography—one of Wong’s earlier inventions—and other existing imaging technologies.
The proton therapy CT couch will integrate radiation simulation with radiation treatment, and because Wong is the inventor, his patented technology will be unique to the Kimmel Cancer Center’s radiation oncology clinics, including the Proton Therapy Center.
The idea to integrate imaging with therapy came to him when he observed colleague Akila Viswanathan’s novel 3D image-guided brachytherapy. One part involves advanced MRI guidance, and the other uses mobile CT to check the placement of the implant every day to confirm the location of the radioactive seeds that treat cervical, uterine and vaginal cancers.
“It made me realize you could do CT guidance with a small footprint,” he says. This small footprint makes it possible to bring imaging into the treatment room without interfering with the treatment equipment.
“This is precision therapy in practice,” says Theodore DeWeese. “Patients’ tumors are in their bodies in a specific orientation, and this differs patient by patient.” One size doesn’t fit all, he explains.

We have to target each patient’s cancer differently, and we do this based on a sophisticated set of scans before patients are treated. Those images are fused together, sort of like virtual reality, so we know precisely where in the body the tumor is in relationship to the normal cells around it.
- Theodore Leslie DeWeese, M.D., Department of Radiation Oncology and Molecular Radiation Sciences
DeWeese says a CT of patient is done to see where cancer is on the day of treatment relative to where it was determined to be in treatment planning. All of the images are merged to precisely aim the beam within an incredible one-tenth of 1 millimeter accuracy.
The CT couch will be integrated into both photon and proton therapy, helping ensure the treatment beam goes where it is intended, and perhaps more importantly, avoiding critical organs and structures that need to be protected from radiation treatment.