A decade ago, insurance rarely covered in vitro fertilization (IVF) for couples who weren’t heterosexual, married, and trying to conceive for at least a year. But the landscape has changed significantly since then, expanding coverage and bringing more and more patients in the lesbian, gay, bisexual, transgender, and queer or questioning (LGBTQ) community into the clinic for fertility services, says Katherine Cameron, a reproductive endocrinology and infertility specialist and director of third-party reproduction at the Johns Hopkins Fertility Center.
“A growing number of same-sex, transgender and single parents by choice are coming to Johns Hopkins to build their families,” she says. “They’re some of my favorite people to work with.”
Cameron explained that compared with heterosexual couples, same-sex couples often have many additional choices to make as they plan their fertility journey. For example, in female same-sex couples, both women may have the option to carry, necessitating discussions over which partner might want to be pregnant first. Because these couples also need a sperm donor, they must choose whether they want to use an anonymous donor from a sperm bank or a known donor — often a friend of the couple or a relative of the nongestational partner. They often must also decide which characteristics they want or need the donor to have.
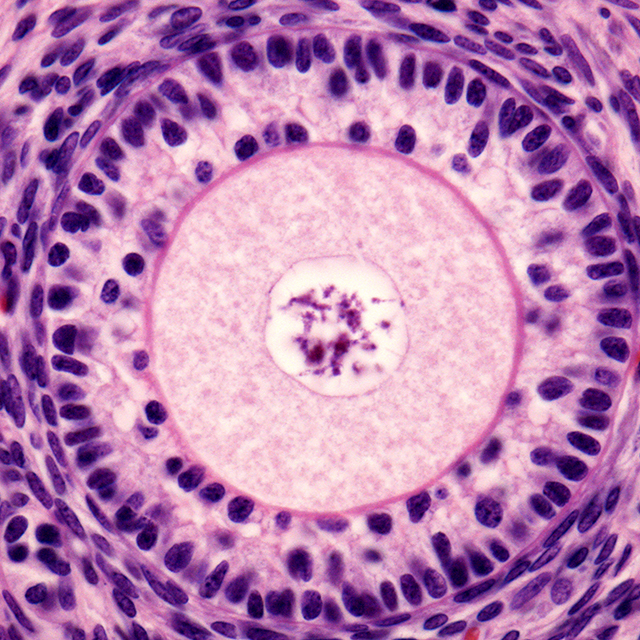
In addition, couples are often faced with options heterosexual couples rarely consider. For example, beyond more commonplace procedures, such as intrauterine insemination or IVF, female same-sex couples can choose an arrangement called reciprocal IVF, in which one partner carries embryos made from the other partner’s eggs. Thus, rather than just one person being the patient, Cameron says that she and her colleagues at the Fertility Center care for both people from different perspectives: one is evaluated and treated for the capacity to produce eggs with hormone stimulation; the other, to maximize the ability to safely and successfully gestate.
Male same-sex couples also seek treatment at the center to create embryos with donor eggs and for help finding a gestational carrier. Another population seen increasingly at the clinic is couples where one or both members are transgender. After these patients transition, many still want to use their own gametes to grow their families. As a relatively new subfield of fertility medicine, Cameron says, transgender care has evolved quickly over time. For example, while she and her colleagues had required female-to-male transgender patients to abstain from their gender-affirming hormones for three months before gamete collection, newer data suggests that patients can typically stay on testosterone throughout their treatment.
Because many couples decide to have more than one child, Cameron says she often works with the same families over time through multiple pregnancies.