Johns Hopkins neurologist Ellen Mowry is using an abundance of data to figure out what therapies will work best for different groups of patients with multiple sclerosis. It’s a daunting task: The neurological disease not only varies greatly in how quickly it progresses but also in how much it debilitates patients.
After identifying patient subgroups based on projected disease progression and other characteristics, the associate professor of neurology and epidemiology hopes to determine which patients are at risk for long-term side effects from particular medications. Another aspect of this research is establishing when those drugs’ potential for healing outweighs the risk of harm.
“In the MS field, this really has great potential to help us stop considering a one-size-fits-all approach and think about patient-specific treatment,” Mowry says.
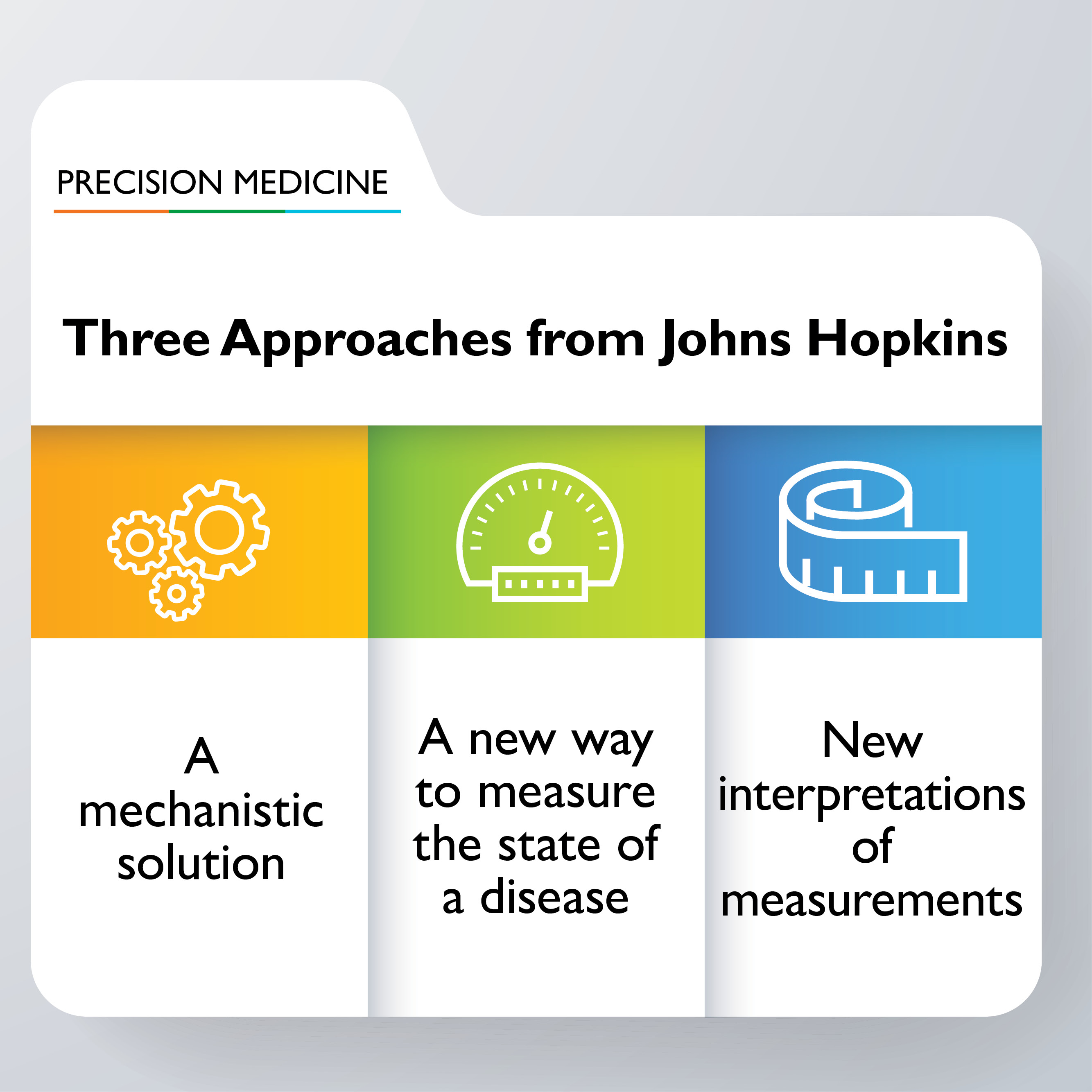
Her work is an example of how precision medicine is bringing researchers closer to tailoring treatment to patients’ specific needs. Defining subsets of patients, then determining the best therapies for them, is one way Johns Hopkins Medicine seeks to improve health care while cutting its costs, according to Antony Rosen, vice dean for research and director of Johns Hopkins inHealth, the institution’s precision medicine effort.
A symposium on May 30 will highlight some of the projects underway, and point to new tools and strategies to make precision medicine available to more researchers across Johns Hopkins.
“The way we do research is dramatically changing because the quantity of data we can collect on individuals and populations is truly massive,” says Dwight Raum, vice president and chief technology officer for The Johns Hopkins University and the Johns Hopkins Health System. “Then we can take what we learn and practice it at a scale that we couldn’t previously contemplate.”
The symposium will feature panels with experts from Johns Hopkins and elsewhere. Discussions will explore how to define patient subgroups by using genetics and genomics and such measurements as imaging. Clinicians and researchers will also detail the approach and practice of precision medicine at Johns Hopkins Medicine and beyond — a conversation that will include officials from the Walter Reed National Military Medical Center and the U.S. Air Force Medical Service.
The event marks the rollout of the Precision Medicine Analytics Platform (PMAP), which uses the cloud — a secure online network of software and services — to collect and interpret individual patient data gathered from genetic information and other sources, along with the larger body of knowledge on particular diseases. PMAP has been piloted by researchers in prostate cancer, MS and other diseases.
Kenneth Pienta, director of research at the James Buchanan Brady Urological Institute, says precision medicine and PMAP have already changed the way patients are treated for prostate cancer at Johns Hopkins. Using data collected from patient subgroups since 1995, Hopkins urologists are better equipped to predict disease progression in patients and determine the course of their treatments.