When Mattan Schuchman got a phone call that one of his patients had fallen, that his ankle was swollen and that he was in a lot of pain, the Johns Hopkins physician quickly arranged for an X-ray technician to make a house call.
While most patients would go to an emergency department or schedule an office appointment, 78-year-old Arthur Cate required the home visit. Seven years ago, the East Baltimore man suffered two strokes, and he struggles with chronic obstructive pulmonary disease (COPD), making it hard for him to leave the house.
Luckily, Arthur didn’t have a fracture, and his ankle healed with elevation, compression and over-the-counter anti-inflammatory drugs.
House visits such as this, and the help of his primary caregiver — his wife, Christina, 57 — help Arthur stay out of the hospital and maintain his level of health.
Schuchman is medical director of Johns Hopkins Home-Based Medicine (JHOME), a primary care program based in Baltimore through which he sees patients age 65 and older who have trouble leaving their home due to chronic conditions such as arthritis, heart failure and dementia.
“Even though Christina is able to get Arthur down the stairs, it would be a monumental effort for her to get him to a doctor’s appointment,” Schuchman says. “Just being 78, but also having two complex chronic conditions, he would need to come in for appointments relatively frequently. The program is really significant for relieving the burden of caregivers.”
Schuchman, along with JHOME nurse practitioners, see their patients about six to eight times each year. If urgent issues come up, such as problems with urination (common in bedbound patients) or trouble breathing (Arthur’s COPD acts up during Baltimore’s humid summer months), JHOME can generally treat patients within 24 hours.
A Life-Changing Stroke
The Cates were living in southern Pennsylvania in April 2012 when Arthur had a mild stroke, followed by a severe one that caused him to be hospitalized for a week at Johns Hopkins Bayview Medical Center. Inpatient rehabilitation took another two weeks. Because the couple had a home in East Baltimore, Christina was able to walk back and forth to the hospital to visit her husband.
Once Arthur was discharged, Johns Hopkins Home Care Group (JHHCG) provided 60 days of physical, occupational and speech therapy at home. Since then, he has been hospitalized for a kidney infection and twice for pneumonia. JHHCG, which with JHOME is part of Johns Hopkins Home & Community-Based Services, also provided therapy services after two of those hospital stays.
Because the stroke greatly affected his right side, Arthur now spends most of his time in bed on the second floor of the house. His wife bathes him, clothes him and prepares his meals. He comes downstairs for dinner using a stair lift, and the couple often watches TV together afterward. Christina is grateful for JHOME.
“It is so much easier on the caregiver and the patient, especially for people with weaknesses on their sides,” she says. “It’s just so hard and exhausting for him to get out.”
Because Arthur’s speech is hard to understand, Schuchman starts his medical visits by checking in with Christina. He then goes upstairs to speak with and examine Arthur.
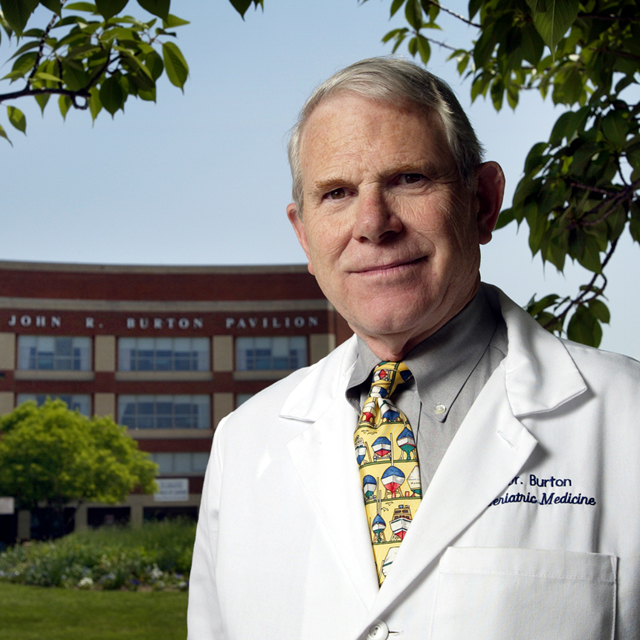
On some visits, Schuchman accompanies an internal medicine resident who leads the checkup. The program is a fertile training ground for learning about medicine outside of a typical clinical setting, and house calls are part of a primary care track program for internal medicine residents at Bayview. Formerly known as the elder house call program, JHOME was started in 1976 by John Burton, former director of the Division of Geriatric Medicine and Gerontology. (See sidebar)
The JHOME staff includes two nurse practitioners who do home visits, a social worker, a nurse case manager and a community health worker. Schuchman began at JHOME during a fellowship in 2015, and became a part-time faculty member at the Johns Hopkins University School of Medicine upon graduating in 2016. But he says he realized the need for such care earlier when his wife’s grandmother, while in her 90s, developed a debilitating heart condition.
“Observing her struggle with getting adequate medical attention, and the lengths our family had to go to for her to reach her medical appointments, inspired me to provide this care to others,” he says.

A Hands-On Caregiver
Christina Cate says taking care of her husband full time seems natural to her.
“I took care of my mom from the time I was 11 until the time I was 18. She had emphysema, so she was on oxygen 24/7,” Christina says. “People say to me, ‘How can you stay so positive?’ I’ve always been a caregiver.”
Aides from the U.S. Department of Veterans Affairs provide relief three times per week, helping Arthur with meals and sitting with him so Christina can leave the house.
“You need that break as a caregiver,” she says. “You can burn out really quick.”
Since becoming a round-the-clock caregiver, she has also become an advocate for those in similar circumstances.
As a member of the patient and family advisory council serving JHOME and JHHCG, Christina helped create a resource guide that The Johns Hopkins Hospital and Bayview use to help ease the transition from hospital to home for patients with complex conditions. The checklist for patients and caregivers includes advice on what medical and cleaning supplies are necessary, how to manage medications and other aspects of home care.
(Christina says she didn’t know she would need extra-large twin sheets for the hospital bed at home, or that it should be near an electrical outlet. That information, for instance, is in the resource guide.)
Because most homebound patients have an advanced disease, the average prognosis for a JHOME patient is two years, Schuchman says. Arthur has now been treated at home for five years.
Schuchman thinks Christina’s diligence has played a major part in her husband’s longevity.
“I think his case is a particular testament to how well patients can do and how dependent their health outcomes can be on their caregivers,” he says. “I think the reason that he’s been successful, living somewhat independently at home, is because he has such a wonderful, conscientious caregiver.”