Amit Jain is on the forefront of spine surgery innovation as an early adopter of minimally invasive lateral access and robotic spine surgery, or MILARS. “This specific combination of technologies — lateral access and robotics — has the potential to change our field, to move the entire field of spine surgery forward,” says Jain, chief of minimally invasive spine surgery and assistant professor of orthopaedics and neurosurgery at Johns Hopkins. “This innovative technique can really provide significant benefits to our patients.” Jain is part of a team of Johns Hopkins surgeons, including Jay Khanna, Khaled Kebaish, and Nick Theodore, who are developing clinical and research protocols for this combination of procedures.
As opposed to traditional open spine surgery, which involves extensive muscle manipulation, MILARS uses a different approach. “Lateral access allows us to perform spine surgery in a way that is frequently muscle sparing, which has profound implications for recovery. You can substantially minimize blood loss and the duration of hospital stays because it is not as disruptive of the physiology of the body,” Jain says.
Lateral access spine surgery allows for indirect spinal decompression, which avoids the nerve irritation that may occur with direct manipulation. These aspects combined make the procedure more efficient in terms of operating room use. “You can accomplish a goal very quickly. For example, you can perform a lateral access surgery with robotic screw placement in less than an hour, as opposed to an open approach that could take several hours,” Jain says.
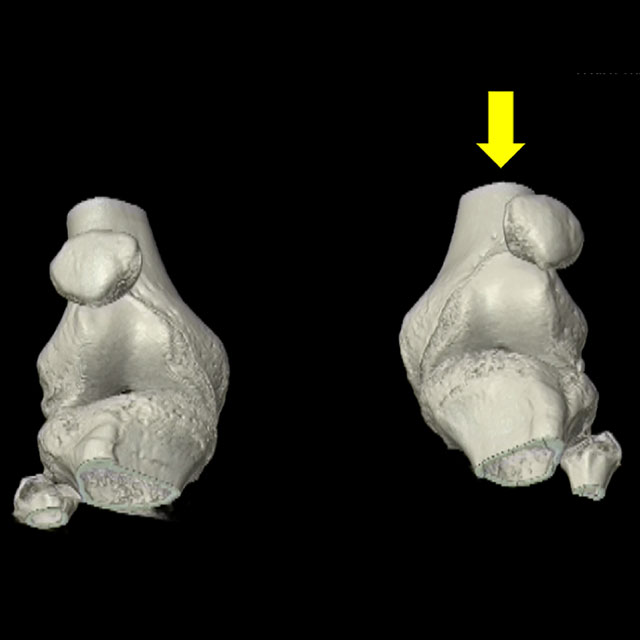
MILARS relies on a state-of-the-art robotics navigation and guidance system, which was approved by the FDA in 2017. Surgeons can use the robot to guide pedicle screw placement. “It’s precision medicine,” Jain says. “With robotics you can, in a very accurate manner, instrument the spine, making the operation safer for the patient.”
The ideal patients for this combination of techniques are those with a focused problem in one, two or three spinal levels. Patients with spondylolisthesis, foraminal stenosis or lumbar spinal stenosis can benefit greatly from MILARS. Other indications include adjacent segment disease and degenerative scoliosis.
Jain also sees the potential for major savings in health care resources. “More than a quarter million lumbar fusions are performed in the country each year, and if perhaps a fifth of them can be performed with MILARS, the reductions in blood loss, morbidity, intensive care unit stays, and hospital stays would have a substantial impact,” Jain says.
Patients will appreciate the benefits, as well, he says. “Patients love having faster recovery, better outcomes, smaller scars and the ability to go home the next day instead of a week later.” For many patients, the difference in recovery time would make traveling to Johns Hopkins, even from far away, worthwhile. “We are among a handful of surgeons nationally that combine lateral access surgery with robotic spine operations. At Hopkins, we could provide a fundamentally different surgical experience with MILARS than that of the traditional method available at local community hospitals,” he says.
Jain has published over 130 peer-reviewed journal articles focused on improving outcomes of spine care.