Conventional rehabilitation usually focuses on one area of physical function, such as the way a person walks or how they use their hands. At the Johns Hopkins Precision Rehabilitation Center of Excellence, physicians, researchers and clinicians focus on multiple facets of function and emphasize a “whole-person” method.“Our approach is unique because we are calling for in vivo measurements of physical, cognitive and psychosocial function to inform personalized interventions,” says Stephen Wegener, co-director of the center of and a researcher in the Johns Hopkins Department of Physical Medicine and Rehabilitation.
Supported in part by Johns Hopkins inHealth — which is comprised of a team of Johns Hopkins clinician-scientists, engineers, health care informaticians and software engineers — the center has developed several technologies to collect, store and analyze data on tens of thousands of patients.
“We’re combining large-scale electronic health data that we already have with longitudinal, prospective data to get the whole picture of how a person is doing,” says Ryan Roemmich, a human movement researcher in the Department of Physical Medicine and Rehabilitation and the Kennedy Krieger Institute. “It’s comprehensive, and we have the ability to do it at scale with automation and centralization.”
To gather measurements of physical function, such as heart rate and step count, the team developed software that automatically requests and collects the measurements from a wearable device. The same application gathers results from periodic, standard assessments of cognitive and psychosocial function.
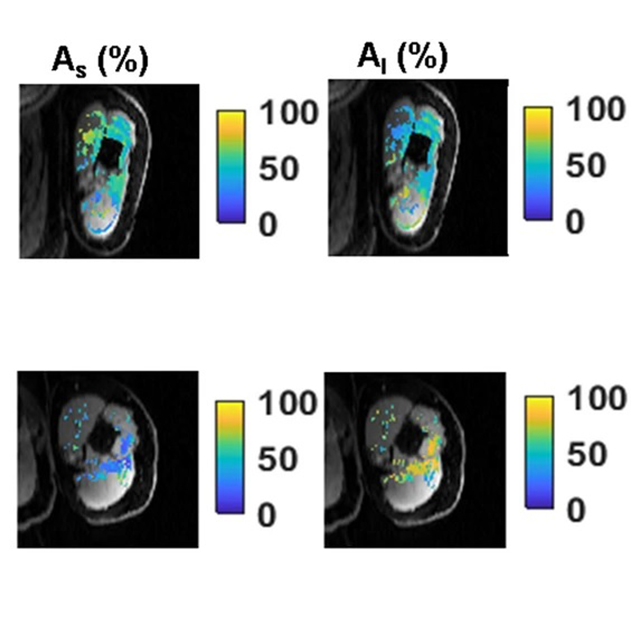
The group also leverages a program to measure body movements from video recorded by a smartphone. The measurements produce quantitative data that can be used to track changes over time.
“As we try to find paths toward patient-specific care, we have these data sources that we can look at simultaneously to identify subgroups of patients who require similar rehabilitation,” says Roemmich. “Without this data, the subgroups wouldn’t even be noticeable.”
The measurements are delivered to a HIPAA-compliant database, where they are stored alongside information from the patients’ electronic health records. So far, data has been amassed on 14,000 patients who’ve experienced stroke and 40,000 patients who have chronic obstructive pulmonary disease (COPD). Johns Hopkins researchers are analyzing the data to identify patients with comparable functional profiles. Their aim is to see who would likely benefit from similar rehabilitation interventions designed specifically for such patients.
In the future, it is hoped, the work will be applied to make individualized predictions in electronic health records that clinicians can review.
Pablo Celnik, co-director of the Johns Hopkins Precision Rehabilitation Center of Excellence, says there is a lot of excitement about precision rehabilitation.