Radical Innovator
Patrick Walsh’s development of the nerve-sparing prostatectomy forever changed the grim outlook for men with prostate cancer. Looking backs, he says the discovery hinged on a key moment: listening to his patient.
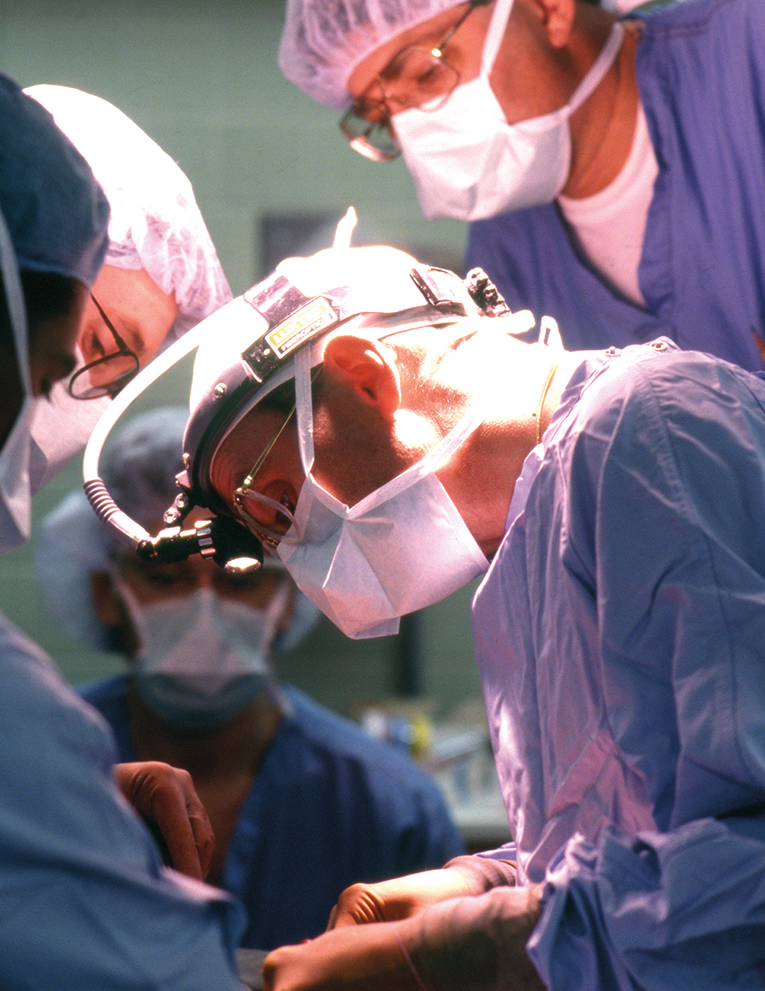
Patrick Walsh in surgery in 1991. Credit: Courtesy of the Alan Mason Chesney Medical Archives.
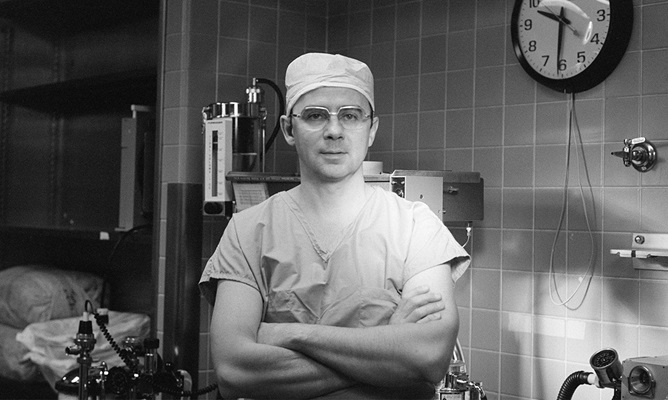
When Patrick Walsh, then just 36, arrived at Johns Hopkins to head up the Brady Urological Institute, prostate cancer often carried a death sentence. This was in 1974, the era before prostate-specific antigen (PSA) blood testing, which today is widely used to screen for prostate cancer early on, when it is still treatable. Even patients who had potentially curable disease were rarely treated with curative intent, as radiation therapy had not yet sufficiently advanced. Surgery — the radical prostatectomy pioneered in the early 1900s by Johns Hopkins’ own Hugh Hampton Young — was widely considered worse than the disease itself.
That’s because 100% of men who underwent a radical prostatectomy became impotent, explains Walsh, today University Distinguished Service Professor of Urology Emeritus.
Roughly 25% experienced severe urinary incontinence. Few surgeons even wanted to undertake the surgery because of the massive bleeding that occurred when operating.
In the early 1980s, Walsh forever changed the grim outlook for men the world over when he developed a surgical approach that became known as nerve-sparing radical prostatectomy. The technique allowed surgeons to excise the cancer while preserving a man’s potency and urinary continence.
After completing the first purposeful such surgery on April 26, 1982, Walsh would go on to refine his technique while performing nerve-sparing surgeries on thousands of men at Johns Hopkins and beyond over the next three decades.
As Walsh recalls his journey to discovery today, he says the path to transforming the care of men with prostate cancer hinged on a key moment: listening to his patient.
‘Where Were the Nerves?’
Walsh’s nerve-sparing innovation was built on an earlier breakthrough. Intent on improving the “problem with bleeding” in prostate surgery during the late 1970s, he zeroed in on the veins surrounding the prostate by using the operating room at Johns Hopkins as his anatomy lab. At this point, he explains, “the veins that caused the bleeding had never been charted, the location of the nerves responsible for erection was unknown and the muscles for urinary control were incorrectly identified.”
Walsh identified a common trunk of veins over the urethra, leading him to a technique that dramatically reduced blood loss, providing a safer and more thorough prostate cancer operation. Soon after using this technique, Walsh says, a Johns Hopkins patient returning for follow-up from prostate cancer surgery announced that he was fully potent.
How could that be? “At that time, everyone believed that the nerves that controlled erectile function ran through the prostate, and it would be impossible to preserve potency,” Walsh recalls. “But from this one patient, I knew that this was not true. But where were the nerves? The answer was not available in any textbook.”
A Chance Encounter
Within weeks of that patient encounter, Walsh attended an international urological conference with his wife, Peg. At a dinner downtown the night before the conference, he noticed an older man about to be seated alone. “For the first and only time in my life, I went up to a total stranger and asked if he would like to join us for dinner, and I asked why he was in town,” Walsh recalls.
The man was Pieter Donker, chair of urology at the University of Leiden in the Netherlands, and the trio enjoyed a dinner together. Four years passed — a time during which Walsh continued to investigate the nerve mystery evoked by his potent patient.
Donker was retired at this point, but his successor invited Walsh to attend a surgical congress in Leiden. On the last day, Walsh’s 43rd birthday, “My host told me that Dr. Donker appreciated my kindness a few years earlier and wanted to return the favor by taking me to see the windmill museum in Leiden.” When the two met up, Donker mentioned that in retirement, he was working in an anatomy lab. Walsh suggested they abandon the museum tour and go to the lab instead, where Donker was dissecting nerves to the bladder in a stillborn baby.
Once there, “when I asked about the location of the nerves responsible for erections,” says Walsh, “he said he had never looked.” The two got to work. “Three hours later, there they were, outside the prostate.”
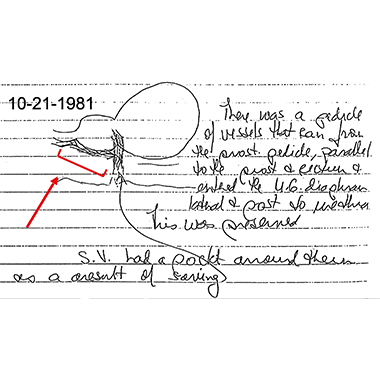
Returning to Johns Hopkins, Walsh in 1981 found that there were vessels located in the exact site where the nerves were present in the fetal dissections. “I speculated that these vessels might provide the scaffolding for these microscopic nerves and could be used as the macroscopic landmark to identify them in the operating room,” he explains.
Using that technique, Walsh performed that first nerve-sparing radical prostatectomy on a 52-year-old man in April 1982. The patient would go on to live a normal life, cancer-free.
Building the Nerve-Sparing Road Map
Over the next decade, urologists from around the world came to Johns Hopkins to watch Walsh perform the radical prostatectomy, which became the most common form of treatment for localized prostate cancer in the United States.
In order to guide that surgery, Walsh needed to confirm the anatomical landmark (or “neurovascular bundle”). He enlisted Johns Hopkins resident Herbert Lepor ’79.
Lepor’s task? To trace the nerves responsible for male sexual function throughout the pelvis. Lepor recalls paying a visit to the Maryland State Anatomy Board on Baltimore Street, where he carefully removed the organs of the pelvis from a cadaver and subsequently worked closely with pathologists at the Armed Forces Institute to create 700 stained sections. These were used by medical illustrators (including Ranice Crosby of Johns Hopkins’ Department of Art as Applied to Medicine) to create a 3D reconstruction.
Says Lepor, “Our reconstruction validated the course of these microscopic nerves as they traversed the pelvis, going alongside the prostate to the penis,” providing a road map for surgeons to reference in their effort to preserve sexual function.
Walsh tapped Lepor to present a poster about the team’s findings at the next American Urological Association meeting. It was a heady experience. “Here were these chairs from departments from all over the country, standing on tables to get a look at what this little resident was saying,” says Lepor, who has gone on to a long career as chair of urology at New York University’s Grossman School of Medicine.
To broaden the findings, Walsh turned to Johns Hopkins resident Peter Schlegel. “With Dr. Lepor’s work, we had information from one cadaver, and we weren’t sure how representative it might be,” Schlegel recalls. Over the next several months, working in the basement of the Marburg Building at Johns Hopkins, Schlegel completed dissections on 10 different pelvises. “It was delicate work. Each dissection could take 10 or 20 hours to complete,” he recalls.
Throughout the painstaking dissections, Schlegel took detailed photos of his work, which he shared with Leon Schlossberg, a faculty artist in the Department of Art as Applied to Medicine. “Leon did a spectacular job” with the resulting seminal medical illustration, says Schlegel.
Today, a framed copy of that illustration hangs on Schlegel’s office wall at Weill Cornell Medicine, where he chaired the Department of Urology. “For more than 20 years, as I was doing radical prostatectomies, I referenced the illustration in the OR with my residents,” says Schlegel. “After surgery, I would bring them back to my office to see it.”
“For more than 20 years, as I was doing radical prostatectomies, I referenced [Schlossberg’s] illustration in the OR with my residents. After surgery, I would bring them back to my office to see it.”
Peter Schlegel
Crucial Conversations with Patients
Between 1982 and January 2011, when Walsh performed his last surgery, he completed nerve-sparing prostatectomies on 4,569 patients. “I spoke to every one of those patients every three months in the first year after their surgeries — that was more than 18,000 telephone conversations,” he says. Those conversations guided him to further refine his surgical technique and improve quality of life measures, Walsh says. Also critical were videos he made of these surgeries, which he examined frame by frame to identify slight variations that enhanced recovery. “I made 28 changes over those 29 years,” says Walsh.
In 2004, he produced a detailed DVD of the operation. With support from the Mr. and Mrs. Robert C. Baker Family Foundation, he distributed 50,000 copies worldwide free of charge to all urologists who sought one.
Walsh’s acolytes in prostate surgery — notably the 62 residents who trained under him during his three decades leading “The Brady” — carried his transformative technique out into the world. Twenty-three of them, like Lepor and Schlegel, became directors of leading urology departments around the country.
At the time Walsh stopped operating, 93% of his patients who underwent nerve-sparing prostatectomies reported being potent at 18-month follow-up. And 95% had total urinary control. “These results were far, far different from when I began my journey,” he says.
Urology’s Influencer
Patrick Walsh served as editor of Campbell’s Urology, the 4,000-page “bible” of urology, for 25 years. In 2012, it was renamed Campbell-Walsh Urology in his honor. In 2023, Walsh was identified as the most cited urologist in the world.
