As a palliative care doctor, Nathan Gray helps patients navigate some of the most intimate and wrenching moments of their lives. As a graphic medicine artist, he distills such complexities into comics that engage millions in such publications as the Los Angeles Times and Washington Post.
The two roles reinforce each other, says Gray, assistant professor of palliative medicine at Johns Hopkins Bayview Medical Center.
His clinical work makes him a better artist by providing an intimate window into stories of life, love and the occasional ironies of giving and receiving care in the American health care system. And his art makes him a better doctor, he says, by constantly reminding him to truly hear his patients’ stories and keep an open mind.
Palliative care is complicated and often misunderstood, Gray says. It encompasses a broad spectrum of symptom and pain management for people with serious illnesses, even alongside care aimed at cure or recovery. Hospice, which typically provides comfort-focused care after curative treatments have stopped, is often confused with palliative care, but is just one aspect of it.
While Gray’s patients may be at many different points in their diagnosis, all wrestle in one way or another with the effects of serious illness and its impacts on their life physically, emotionally, and socially. His job, he says, is to help them and their families navigate the experience, manage symptoms, and make sure that the care they are receiving matches their goals and values. It’s not easy.
“I’ll never fully be able to understand what the patient is experiencing. But I try to listen without judgement, to learn who they are and what matters most to them,” he says.
“I think we all have our biases about what we would choose if we were on other side of the bed rails in a difficult situation. Everything from, ‘I’d want that machine’ or ‘I don’t want that machine’ at the end of life, to ‘I’d rather hurt than take that opioid because I’m worried about side effects.’ Sometimes those decisions don't seem to make sense to us doctors in the in the heat of the moment, but might make sense later if we're in those shoes or in that hospital gown.”
He says he loves the opportunities that palliative medicine provides to learn more about the lives his patients live, such as favorite pets or hobbies. He always asks long-time couples for their advice about making love last.
The answers to this last question became one of Gray’s recent pieces, which ran in the Washington Post on Valentine’s Day, 2023, under the headline, “Lifelong Couples Told Me their Secrets. This is What they Said.”
In 11 panels hatched in pink and blue pencil, Gray pokes gentle fun at the “vague and unsurprising” answers he usually gets, and notes that couples often have no idea how they’ve stayed together for so long, or disagree about the strategies that worked for them.
In one panel, a man says “we’ve never had a true fight,” while the woman says, “we bicker constantly.”
David Wu, director of palliative care at the Johns Hopkins Bayview Medical Center, wholeheartedly agrees that the arts can make palliative care doctors better at their jobs. “They are a way for us to get a deeper connection to each other, to equip us to wrestle with uncertainty and the big questions around death, love, loss and grief,” he says.
Wu, an English major at Yale University, developed the 3-Act Model, an approach to communication training that uses reflection on poetry and other narrative tools to help healthcare providers develop care plans with patients. The program’s three-act structure starts with a clinician listening to and understanding a patient’s story, then moves to a second act of discussing medical options before concluding with third act of making shared decisions based on both the patient’s values and the medical situation at hand.
This curriculum, which is integrated in multiple training programs and units for a variety of specialties, was recently recognized when Wu and his palliative care team won a 2022 award for Innovations in Clinical Care from Johns Hopkins Medicine.
Wu also plays guitar, and when he saw one of Gray’s previously published works, “Dying Words Aren’t What I Imagined,” he asked if he could put the piece to music. The resulting three-minute, 40-second film moves from one of Gray’s still images to another, accompanied by Wu’s haunting acoustics.
In one panel, a man sits up in bed, his mouth a resolute line and his arms folded against the world. “Facing death leads many folks to show superhuman grace,” Gray writes. “But some still hold very human grudges.”
Wu particularly admires Gray’s “thoughtful and nuanced” approaches to difficult topics. “He lands on person-centered care, the need to prioritize patients and people,” Wu says.
For example, one recent Gray piece took on the thorny ethical issues surrounding for-profit hospice centers. Appearing in the Los Angeles Times on Feb. 5, 2023, “Op-Comic: The Perils of a Profit Motive in Hospice Care,” distills a complex idea into 12 densely worded and illustrated panels (plus one for sources), concluding that “The needs of patients shouldn’t be pitted against the pressure for profits.” (See more of Gray’s work on his website, The Ink Vessel.)
For difficult topics, Gray says, he makes sure multiple readers, both medical colleagues and lay people, comment on his comics before he sends them to a publication. “I want to make sure that what I'm saying is sensitive, that it’s accurate, and that it’s accessible from both the medical and lay perspectives,” he says.
The Many Roles of Graphic Medicine
British doctor and artist Ian Williams, who coined the phrase in 2007, describes graphic medicine as a “handy term to denote the role that comics can play in healthcare.” Graphic medicine can raise public awareness, educate trainees, and help patients understand their illness.
Gray recently teamed with second-year medical student Oscar Li to write a book chapter, currently in press, titled, “Drawn Together: Merging Health and Comics Through Graphic Medicine,” for a Biomedical Visualization book series by the Springer publishing company. In it, they discuss a broad range of works considered part of the spectrum of graphic medicine, such as first-person illness memoirs, academic papers, opinion pieces, public health education, and more.
In their chapter, they note that comics have a particular ability to reach readers because they communicate through both words and images.
Li, who minored in animation at the University of Southern California, was able to use his artistic skills to bring public attention to hearing loss, working with otolaryngology professor Frank Lin to create an animated documentary, “What Did You Say?” for the Johns Hopkins Cochlear Center for Hearing and Public Health, which Lin directs.
The seven-minute film combines Li’s drawings with the voices of real people describing their hearing losses. It was created to raise awareness for the center’s Know Your Hearing Number campaign, which seeks to create a single metric for understanding hearing and how it changes over time.
Graphic medicine can help people navigate some of life’s toughest situations, sometimes by reminding them that they’re not alone.
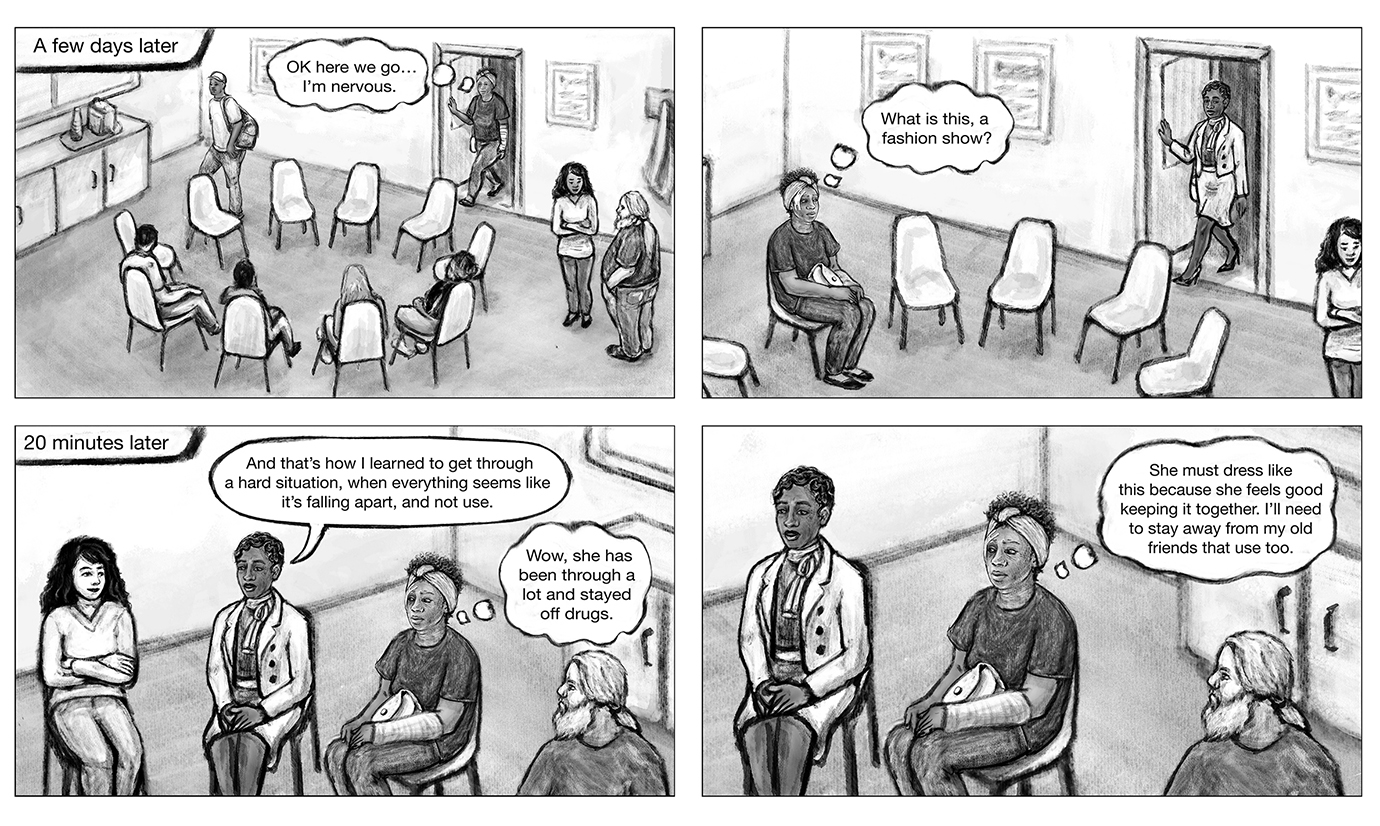
Lydia Gregg, associate professor in the school of medicine’s Art as Applied to Medicine department, spent months creating the stories of Eva and James, fictional people with very realistic substance use disorders. Eva struggles to raise a child and hold a job. James is unhoused and very attached to his dog.
Their experiences turning their lives around with the help of peer mentors and medication are documented in words and images that are available on an app that clinicians and peer mentors can use with patients with opioid disorder.
Oluwaseun Falade-Nwulia, assistant professor of medicine, is leading the effort to develop and assess the app, called mTools4Life, that lets users either scroll through and read on their own or watch as a video with a voiceover.
“Presenting information in visual and narrative form is known to be very persuasive,” Gregg says. “A vivid story with relatable characters can put you in a state of mind where you’re more open to change. Seeing someone like themselves succeed in the stories might help a patient make the leap to start treatment for opioid use disorder.”
Starting a Conversation
Gray, who grew up in Southern California and Tennessee, knew from a young age he was interested in both art and medicine. He didn’t realize until later that the two could intersect in such rewarding ways.
“When I was a kid, I spent a lot of time drawing,” he says. “I wasn’t that serious about it, it was just a wonderful form of creativity and expression. When college hit, I got busy with pre-med courses and then medical school and residency. I picked it back up at the end of residency and I realized that I had missed it a lot.”
Gray went to the University of Texas Southwestern Medical School for medical school and an internal medicine residency, then the Duke University Medical Center for fellowship training in hospice and palliative medicine. “I really liked the role of palliative care in alleviating suffering and the meaning that seemed to infuse each day when you were taking care of people who are seriously ill,” he says.
He joined the Duke faculty in 2014 and came to Johns Hopkins in January 2022 with his wife Bethany Gray, assistant professor in the Department of Pharmacology and Molecular Sciences.
“One thing that I really like about comics is that they’re a great medium for starting a conversation,” he says. “I generally make comics that are short and pretty quick to read, while at the same time, trying to tackle complicated subjects in a way that’s engaging and colorful. Comics can draw people into something that they might not necessarily read as a text article, either because the topic seems too dense, or maybe because it feels a little scary.
“A comic can bring people in.”



